Printer Friendly Version in PDF Format (55 PDF pages)
ABSTRACT
Many women facing opioid addiction are either pregnant or caring for children and face a number of social, structural and economic barrier in accessing treatment. In recent years, clinicians and policymakers have become increasingly interested in supporting substance use treatment approaches that provide comprehensive services to pregnant and parenting women and their family members and recognized the women's role as primary caregivers. Since MAT is the recommended clinical practice for treating pregnant women and adults with OUD, we sought to define how MAT can be combined with family-centered services. This study further examined a selection of state and local treatment programs targeted to pregnant and parenting women and their families to identify key challenges and opportunities in expanding access to comprehensive, family-centered services and MAT treatment for this population.
DISCLAIMER: The opinions and views expressed in this report are those of the authors. They do not reflect the views of the Department of Health and Human Services, the contractor or any other funding organization. This report was completed and submitted on September 25, 2018.
TABLE OF CONTENTS
1. BACKGROUND
2. METHODS
2.1. Overview
3. FAMILY-CENTERED MEDICATION-ASSISTED TREATMENT PROGRAM FRAMEWORK
3.1. Program Framework
4. SELECT FINDINGS FROM A STATE PROGRAM SCAN
4.1. Statewide Initiatives Versus Standalone Programs
4.2. Eligibility Rules and Requirements Across States
4.3. Care Coordination
4.4. Statewide Initiatives for Capacity Building
4.5. Partnerships
5.1. Overview
5.2. New Hampshire Case Study
5.3. Ohio Case Study
5.4. Pennsylvania Case Study
5.5. Texas Case Study
6. CHALLENGES AND OPPORTUNITIES RELATED TO TREATMENT
6.1. Insurance Coverage
6.2. Funding Constraints
6.3. Workforce Capacity Shortages
6.4. Limited Access to Safe and Affordable Housing
6.5. Provider Reluctance to use MAT
7. ADDITIONAL FINDINGS AND RECOMMENDATIONS
APPENDICES
- APPENDIX A: STATE OPIOID USE DATA
- APPENDIX B: PROGRAM SCAN
LIST OF EXHIBITS
- EXHIBIT 1: Program Framework
- EXHIBIT 2: State Policies Regarding Reporting and Treatment of PPW and OUD Across Selected States
- EXHIBIT 3: Statewide Partnerships for PPW with OUD
- EXHIBIT 4: Key Dimension of MAT Treatment Programs
ACRONYMS
The following acronyms are mentioned in this report.
| ACA | Affordable Care Act |
|---|---|
| AIM | Alliance for Innovation on Maternal Health |
| ASAM | American Society of Addiction Medicine |
| BHA | Maryland Behavioral Health Assessment |
| BSAS | Massachusetts Bureau of Substance Addiction Services |
| C4CS | Maryland Center for a Clean Start |
| CAP | Maryland Center for Addiction and Pregnancy |
| CDC | Centers for Disease Control and Prevention |
| CHARM | Vermont Children and Recovering Mothers |
| CHCS | Center for Health Care Services |
| COE | Center of Excellence |
| CRFTSAR | Kentucky Comprehensive Residential Family Treatment for Substance Abuse Recovery |
| DSHS | Texas Department of State Health Services |
| HRSA | Health Resources and Services Administration |
| KORE | Kentucky Opioid Response Effort |
| MassTAPP | Massachusetts Technical Assistance Partnership for Prevention |
| MAT | Medication-Assisted Treatment |
| MATR | Kentucky Maternal Assistance Toward Recovery |
| MCH | Ohio Maternal Care Home model |
| MCPAP | Massachusetts Child Psychology Access Program |
| MIR | New Hampshire Moms In Recovery |
| MOMS | Ohio Maternal Opiate Medical Supports |
| MOMS+ | Ohio Maternal Opiate Medical Supports Plus |
| Mothers MATTER | Pennsylvania Mothers Medication-Assisted Treatment for Engagement and Resilience |
| MRI | Magnetic Reonance Imaging scan |
| NAS | Neonatal Abstinence Syndrome |
| NFP | Nurse Family Partnership |
| NICU | Neonatal Intensive Care Unit |
| OB-GYN | Obstetrics and Gynecology |
| OHH | Opioid Health Home |
| OTP | Opioid Treatment Program |
| OUD | Opioid Use Disorder |
| PAT | Parent as Teachers program |
| PATHways | Kentucky Perinatal Assistance and Treatment Home |
| PPW | Pregnant and Postpartum Women |
| Project RESPECT | Recovery, Empowerment, Social Services, Prenatal care, Education, Community and Treatment project |
| PTSD | Post-Traumatic Stress Disorder |
| QBHE | Qualified Behavioral Health Entity |
| RTI | Research Triangle Institute |
| SAMHSA | Substance Abuse and Mental Health Services Administration |
| SMARTS | Kentucky Supporting Mothers to Achieve Recovery Though Treatment and Supports |
| SOR | State Opioid Response grant |
| STR | State Targeted Response |
| SUD | Substance Use Disorder |
| UNC | University of North Carolina |
| UPMC | University of Pittsburgh Medical Center |
1. BACKGROUND
Growing rates of opioid misuse and opioid use disorder (OUD) in the United States are often described in terms of overdose deaths, opioid prescriptions, and number of individuals with OUD. While these are valuable metrics that help quantify the problem, they obscure the fact that opioid abuse occurs not within a vacuum, but within families and social networks -- and these families and networks face consequences of addiction alongside the individual. Many women struggling with OUD are either pregnant or caring for children. As of 2005, approximately 70 percent of women entering substance use disorder (SUD) treatment services (for opioid and other substances) had children (SAMHSA, 2007). The National Survey on Drug Use and Health indicates that between 2010 and 2014, 40 percent of all adults with a SUD diagnosis were living with at least one child. Adults with SUD living with children were more likely to be between the ages of 26-50 and to be female compared to the rest of the SUD population (Feder et al., 2018). Further, about one in eight children (8.7 million) aged 17 or younger live in households with at least one parent who had a past-year SUD (Lipari & Van Horn, 2017).
Pregnancy is a particularly critical time to address OUD, as prenatal maternal opioid use is associated with serious complications for the baby including premature birth and neonatal abstinence syndrome (NAS). Women may also be more receptive to seeking treatment during this transitional period of their lives. The rise of the opioid epidemic has corresponded to a rise in NAS, which increased nearly seven-fold between 2000 and 2014 (Patrick, 2018). Furthermore, while the overall proportion of pregnant admissions in the United States remained stable around 4 percent from 1992-2012, admissions of pregnant women reporting prescription opioid abuse increased from 2 percent to 28 percent (Martin et al., 2013).
|
What is Medication-Assisted Treatment (MAT)? MAT is the use of medications in combination with evidence-based counseling and behavioral therapies for the treatment of SUDs. Medications used in treating pregnant women with OUD may include:
For treating pregnant women, less is known about the safety of:
SAMHSA, Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants (2018). |
Given the interplay of addiction, family, and pregnancy, states and programs are increasingly acknowledging the value of providing treatment to pregnant and parenting women through family-centered programs. These programs recognize women's roles as caregivers within the family unit, include their children, partners, and/or other family members in the treatment process, and provide clinical care for all affected family members. In addition to clinical treatment -- which includes use of medication-assisted treatment (MAT) as a best practice for treating pregnant and parenting women -- family-centered programs include a range of supportive and community-based services. These may include child care, transportation, housing, employment training, parenting education, and linkages to financial aid and other human services programs. Family-centered programs incorporating MAT can improve pregnancy outcomes by shielding mothers from the drug use environment and engaging them in a network of support. Family-centered programs also benefit infants by strengthening the bond between the mother and infant, thereby improving infant health outcomes. However, many challenges remain for expanding pregnant and parenting women's access to family-centered programs that incorporate MAT. Issues such as stigma, unstable or unaffordable housing, lack of specialty providers, and lack of funding have been cited as barriers to treatment for women. Provider unwillingness to provide MAT to pregnant women -- either due to lack of credentialing or training in this area, bias, or a combination of these factors -- is also a common barrier.
Nevertheless, a number of states are incorporating family-centered treatment principles into MAT services and supporting innovative approaches to creating relevant clinical and community linkages. This paper explores the core components of a family-centered MAT program framework; provides an overview of state variation in eligibility requirements and care coordination; summarizes four states' individual approaches to treatment; and discusses challenges, barriers, and recommendations for future work in this critical area.
2. METHODS
2.1. Overview
Information in this report draws from three sources: a program scan consisting of an Internet search of state and regional initiatives supporting family-centered MAT for pregnant and parenting women with OUD, key informant interviews representing a variety of perspectives on family-centered treatment of pregnant and parenting women, and a review of relevant literature.
To assist in identifying state initiatives for the program scan, RTI reviewed documents describing family-centered concepts, as well as documents and websites describing relevant programs. RTI used these documents as a starting point to identify states with programs, services, funding mechanisms and policies supporting the identification and treatment of pregnant and parenting women with OUD. To more narrowly focus the search, we focused on the 21 states with women and families most affected by the opioid epidemic. This included the states with:
-
the highest rate of opioid prescriptions per 100,000 persons;
-
the highest levels of female opioid related death; and
-
the highest incidence of NAS.
The findings from the program scan were catalogued, synthesized and included in a separate report, while select findings are provided in this report.
Key informant interviews included researchers, federal and state officials and providers whose work supported family-centered treatment services for pregnant and parenting women with OUD, including MAT. State officials were drawn from agencies in four states identified as supporting programs with elements of family-centered treatment: New Hampshire, Ohio, Pennsylvania and Texas. In these states, where possible, the study team also interviewed provider representatives to gain additional perspective on the service delivery systems. Two provider researchers, nationally known for their research and provision of services to women with OUD and their children, were also interviewed, as were and federal officials supporting treatment programs for pregnant and parenting women with OUD.
An interview guide was drafted based on the primary policy questions to be assessed. Interview questions focused on gaining knowledge of the range of services provided to pregnant and parenting women with OUD; how these services are organized and funded; how states are incorporating family-centered or family-centered treatment principles into these programs; and any barriers and challenges to implementing these types of initiatives. Each telephone interview lasted 60 minutes and was followed by email as needed to verify specific points or to obtain materials referenced in the interviews. Content analysis emphasizing primary policy questions was conducted on the data obtained from the interviews. The findings from the interviews are synthesized and included in this report, while the findings from the state and provider interviews are summarized in this report as case studies.
3. FAMILY-CENTERED MEDICATION-ASSISTED TREATMENT PROGRAM FRAMEWORK
Pregnant and parenting women face multiple legal, social and structural barriers in accessing, and adhering to, treatment. Legal issues women face include the criminalization of opioid use during pregnancy and potential loss of child custody. Many state laws conceptualize OUD as a criminal behavior instead of a chronic disease which prevents women from seeking evidence-based care (Krans & Patrick, 2016). Pregnant women with OUD also face complex social barriers to accessing treatment including stigma and caregiver responsibilities. Finally, structural issues faced by pregnant and parenting women with OUD include treatment issues, workforce issues and lack of social services. Treatment issues include cost of care and limitations in insurance coverage. In particular, Medicaid has higher income thresholds for pregnant women, but the coverage extends only to 60 days postpartum for women who are not eligible through another pathway for Medicaid in the postpartum period. Not all of the states hardest hit by the opioid epidemic have participated in Medicaid expansion which could potentially benefit pregnant and postpartum women (PPW) with OUD when birth benefits run out.
There are multiple workforce issues limiting treatment such as provider bias and reluctance to prescribe MAT to pregnant women and a lack of specialty providers who are knowledgeable in treating pregnant women with MAT. In addition, regulations requiring certification limit providers' ability to prescribe buprenorphine. As of 2016, the maximum number of patients to which waivered providers could prescribe buprenorphine was 275, while most physicians could prescribe buprenorphine up to 100 patients.[1] There is reluctance among providers to obtain a buprenorphine waiver. According to the National Alliance of Advocates for Buprenorphine Treatment, despite extensive recruitment efforts, only about 31,000 of America's 800,000 physicians who have the potential to prescribe buprenorphine have obtained a waiver. Additionally, according to one source only a third of waivered providers actually prescribe the medication,[2] while according to another 40 percent of waivered practitioners have not prescribed.[3]
Social service issues faced by pregnant and parenting women with OUD include unstable housing, inadequate transportation options, poor employment prospects and lack of coordination with social programs such as Temporary Assistance for Needy Families and Supplemental Nutrition Assistance Program. Effective treatment requires a comprehensive care program framework that addresses the complex needs of pregnant and parenting women and their children.
Family-centered treatment options recognize women's roles as caregivers within the family unit, include their children and families in the treatment process and provide family-based clinical care. In addition to clinical treatment, family-centered programs include a range of supportive and community-based services that address many challenges facing women and their families: child care, transportation, housing, employment training, parenting education, linkages to financial aid and other human services programs.
3.1. Program Framework
| EXHIBIT 1. Program Framework |
|---|
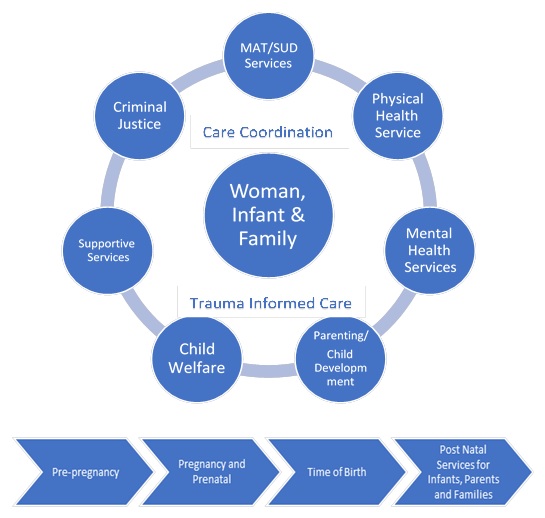 |
In order to order to evaluate state initiatives to provide family-centered services to women, RTI provides a basic framework for family-centered treatment for pregnant and parenting women and their children that includes elements of family-centered care, the American Society of Addiction Medicine (ASAM) dimensions and levels of care, and how MAT can be included. We also include the distinct phases of pregnancy, which can interact with the elements of care. Building upon the dimensions included in the Substance Abuse and Mental Health Administration (SAMHSA) briefings, Family-Centered Treatment for Women With Substance Abuse Disorders: History, Key Elements and Challenges,[4] Perspectives On Family-Centered Care for Pregnant and Postpartum Women: Broadening the Scope of Addiction Treatment and Recovery,[5] A Collaborative Approach to the Treatment of Pregnant Women With Opioid Use Disorders: Practice and Policy Considerations for Child Welfare, Collaborating Medical and Service Providers,[6] and the National Association of State Alcohol and Drug Abuse Directors monograph, Guidance to States: Treatment Standards for Women with Substance Use Disorders[7] and incorporating findings from peer reviewed and grey literature, we present a framework for family-centered services depicted in Exhibit 1. The elements of the framework are described briefly below. This paper aims to describe a family-centered MAT program framework, and not a single model of care. This framework could be worked into a number of different treatment models and approaches that effectively serve populations with OUD, such as those operating under the Medicaid Health Home state plan option and the variety of primary behavioral health integration programs. The "Findings from Interviews" chapter in this report further describes specific models of care implemented in state programs that include family-centered principles.
3.1.1. Central Component of Family-Centered Care
Woman, Infant and Family. In a family-centered framework, pregnant and parenting women, their infants, other children and other family members are the central component of care. Under a family-centered framework, women would be screened, assessed and provided with on-going treatment alongside their family members. Family-centered women's inpatient treatment co-locates the mother with her infant. There is growing evidence that suggests care that preserves the maternal-infant dyad care is beneficial for both the mother and infant (Casper et al., 2014). Co-location of mother-infant services also provides an opportunity for mothers to receive education and support for breastfeeding. Recent research suggests that infants with NAS who are breastfed require less or no MAT, have less severe symptoms, and have a shorter length of hospitalization after birth (Bagley et al., 2014). Non-pharmacological care such as rooming in, swaddling, using pacifiers, breastfeeding and spending quiet time together is a frontline treatment for NAS and might be enough to treat babies with mild withdrawal symptoms (SAMHSA, 2018).
Family-centered residential care serves the pregnant and parenting women with SUD and other children under the woman's care, regardless of age. This is an important aspect of care as it has been determined that women with SUDs, including OUD, who have children are less likely to seek treatment in order to avoid separation and the fear of losing child custody (Wilke, Kamata, & Cash, 2005). Therefore, it follows that residential treatment facilities that provide integrated treatment services for mothers (those that include services such as child care, prenatal care, parenting programs, or allow children to stay with parents in residential settings) show more success than those that do not (Niccols et al., 2012).
Finally, in family-centered care, the concept of family goes beyond the mother-infant dyad to include a family constellation as defined by the woman herself. This inclusive framework may include children, spouses and partners and may also include extended family members and other close members of the community (Dallas et al., 2017). While the SUD treatment field historically sought to provide gender-specific treatment for women, which did not necessarily include fathers or partner parents as a part of women's recovery, family-centered care expands treatment to include fathers and children. This inclusion seeks to make care more comprehensive and sensitive to the needs of women (Davis et al., 2017).
3.1.2. Components of Family-Centered Care
MAT/SUD Services. MAT has been recognized as highly effective in treating individuals with OUD and is recommended as a best practice for treating pregnant women using opioids by the American College of Obstetricians and Gynecologists and ASAM (2012), as well by the recently published SAMHSA guidelines, Clinical Guidance for Treating Pregnant and Parenting Women with Opioid Use Disorder and Their Infants (2018). MAT services should be available for women and their families in all care settings across the ASAM continuum of care: early intervention, outpatient services, intensive outpatient/partial hospitalization, residential/inpatient services, and medically managed intensive inpatient services. For early intervention, outpatient and intensive outpatient services, this may mean development of family goals and inclusion of family members in treatment sessions. For residential treatment, this may mean flexible configurations to include families of all sizes in the residential treatment facility.
For infants, MAT is recommended, in addition to non-pharmacological treatment, when there are symptoms of moderate to severe NAS (SAMHSA, 2018). Research shows that medical intervention to control withdrawal symptoms is required in 27 percent to 91 percent of neonates with NAS (Kocherlakota, 2014). Regardless of setting, in family-centered treatment, the woman and her family are at the center of the treatment.
Physical Health Services/Pediatric Care. Pregnant and parenting women with OUDs and their children often have co-occurring health problems that have not been treated while the woman was under the influence of opioids. In a family-centered framework, physical health services/pediatric care should include primary care; prenatal and postnatal care; emergency/crisis and hospital care; chronic diseases care; and reproductive and sexual health care. Primary care providers should collaborate with specialty providers knowledgeable about MAT utilization during pregnancy and with hospitals regarding delivery policies and MAT practices. Access to family planning services is particularly important for women with OUD. One multi-site, clinic-based study found that 86 percent of pregnancies among women with OUD are unintended versus 45 percent in the general population (Heil et al., 2010).
Mental Health Services. Pregnant and parenting women with OUD are at risk for co-occurring mental health disorders, such as anxiety disorders, mood disorders, personality disorders, psychotic disorders and other disorders. Data from the 2017 National Survey on Drug Use and Health estimate that in the past year 8.5 million adults in the United States had both any mental illness and an SUD, which correlates to 3.4 percent of adults (SAMHSA, 2018). An estimated 3.1 million adults aged 18 or older in the United States had co-occurring serious mental illness and an SUD in the past year, corresponding to 1.3 percent of adults. If unrecognized and untreated, psychiatric disorders can interfere with recovery from OUD.
Pregnant and parenting women with OUD are also at risk for mental health conditions, such as depression and anxiety, which may be the result of sexual assault trauma or domestic violence (SAMHSA, 2018). Family-centered care provides mental health services for the entire family to include a non-judgmental approach to screening, as well as assessment, evaluation, treatment, medications, counseling, cognitive behavioral therapies and other evidence-based treatment. Due to the high percentage of women with OUD and their children experiencing violence and trauma, access to trauma-informed mental health services is key.
Parenting/Child Development. A family-centered framework includes parenting and child development education for the pregnant and parenting women with OUD in order to improve her ability to care for her children. Women with OUD, who may have a history of child abuse often have a need for specialized parenting skills and support. Parenting programs specific for families with SUD such as Celebrating Families, Strengthening Families, and Nurturing Families would be most applicable.
Child Welfare. Many pregnant and parenting women with OUD in treatment are involved with the child welfare system and family courts to determine whether their children may safely remain in their care. Women in treatment may have requirements ordered by the court and monitored by the child welfare agency to maintain their parenting role or to support reunification with children who may have been removed from their care. In a family-centered framework, providers work collaboratively with child welfare and help women meet their requirements to resume parenting responsibilities or to prevent child removal all together.[8]
Supportive Services. Access to safe housing and reliable transportation, with access to schools and child care, are a critical component of treatment for women with OUD and their families. Family-centered treatment provides access to social and community-based services to support women and their families.
Employment. For pregnant and parenting women with OUD, maintaining economic security for themselves and their families is an important component of the recovery process. Often, women with OUD have significant barriers to employment that require specialized employment counseling, job development services or advocacy with employers. A family-centered framework includes access to training and employment services along with child care to enable women to search for jobs and to retain employment.
Criminal Justice. When mothers also are involved in the criminal justice system, linkages and communication with probation and parole staff are critical. Criminal justice requirements may include drug testing, court appearances, and documentation about treatment progress toward goals. Often these communications require access to the community's legal aid services and should include referral to, and coordination with, treatment providers.
A family-centered approach may also include linkages to family drug courts. Family drug courts are designed to be a multidisciplinary, collaborative approach to serve women with SUD and their children who are involved with the child welfare system. Best practice for a family drug court includes bringing in representatives of SUD treatment, child welfare, mental health treatment and social services in order to engage and support the family (Children and Families Futures, 2015).
3.1.3. Embedded Components of Family-Centered Care
Care Coordination Services. Care coordination is an important component of the treatment framework for pregnant and parenting women with OUD that should be embedded throughout programs to support family-centered principles. Care coordination ensures appropriate linkages are made for women and their children and ensures on-going coordination. Care coordination may be provided by professional staff or paraprofessional staff, such as a peer navigator. A peer navigator is an individual with personal experience with SUD recovery and is someone who has had experience "navigating" the SUD treatment service system and can act as a coach and help manage and coordinate care, communicate with providers and provide overall support.
Trauma-Informed Care. A history of abuse or neglect is a risk factor for SUD (Stone et al., 2012). Treatment programs serving pregnant and parenting women serve a high number of women with a history of abuse. One North Carolina residential treatment program reported that at least 80 percent of the women treated come in with childhood or adult abuse (Jones, 2018). Trauma-informed care should also be embedded in a family-centered framework for pregnant and parenting women with OUD. Trauma-informed, or trauma-responsive, care supports a treatment framework that involves understanding, recognizing, and responding to the effects of all types of trauma. Trauma-informed care should emphasize physical and psychological safety for pregnant and parenting women with OUD and their families and should assist women in rebuilding a sense of control and empowerment over their lives and their recovery process.
4. SELECT FINDINGS FROM A STATE PROGRAM SCAN
This section provides key findings from a scan of states supporting programs that offer family-centered MAT for pregnant and parenting women with OUD. We discuss statewide availability of programs, eligibility rules and requirements across states, clinical and community-based services coordination and other themes identified from the program scan.
To narrow the focus of the search, RTI decided to focus on the top 21 states that are heavily impacted by the opioid epidemic with the idea that these states would be more likely to develop state policies providing for the development of family-centered MAT for pregnant and parenting women. RTI developed an algorithm to identify the states with:
-
the highest rate of opioid prescriptions per 100,000 persons;
-
the highest levels of female opioid related death; and
-
the highest incidence of NAS.
The states included in the scan along with opioid prescription data, opioid related deaths and rate of NAS are found in Appendix A.
4.1. Statewide Initiatives Versus Standalone Programs
Most states included in the program scan conducted for this study have standalone specialized SUD programs for PPW with OUD, typically a standalone residential treatment program or intensive outpatient program that services a specific region of the state. However, only one third of the reviewed states have existing statewide initiatives for family-centered treatment for PPW, including access to MAT. Of the 21 states featured in the scan, 11 states (Illinois, Kentucky, Maine, Mississippi, New Hampshire, North Carolina, Texas, Ohio, Pennsylvania, Vermont and Wisconsin) have statewide initiatives that incorporate family-centered treatment either through state amendments, policies, or funding of pilot programs. Six of these 11 states (Kentucky, Maine, North Carolina, Ohio, Texas and Vermont) have family-centered MAT programs specifically for PPW with OUD.
One state, North Carolina, supports a family residential treatment program for women with SUD and their children that is available statewide. CASAWORKS for Families Residential Services consists of 28 programs using evidence-based treatment models located in 13 counties across the state. Family-centered characteristics of the CASAWORKS programs include accommodations for women's children up to age 11, a service array include life skills training, parenting education, child care and transportation, and the ability for women to reside in the program for up to one year. West Virginia is planning to expand their Drug Free Moms and Babies program, an integrated, comprehensive SUD program for PPW from four regional sites to 12 sites across the state. Family-centered aspects of this program include recovery coaches and long-term follow-up for mothers and their babies.
States are using a variety of funding sources to support family-centered SUD services for PPW. Substance Abuse Prevention and Treatment Block Grant funds, Opioid and MAT State Targeted Response (STR) funds, Centers for Disease Control and Prevention (CDC) funding and state funds have been used to support a variety of services to PPW and infants with NAS. A few states have received Section 1115 Medicaid Demonstration Waivers and State Plan Amendments to expand and enhance MAT and other SUD services to PPW and their families. Of note, some states are beginning to take advantage of the new Centers for Medicare & Medicaid Services policy announced in the November 1, 2017, State Medicaid Director's memorandum outlining a more flexible, streamlined approach to accelerate states' ability provide a targeted response to OUD.
A few states are beginning to use 1115 waivers to enhance services to PPW with OUD. For example, in Kentucky, the KY HEALTH (Helping to Engage and Achieve Long Term Health) 1115 Medicaid expansion waiver supports the Kentucky Opioid Response Effort (KORE) which includes services to PPW for 60 days after the pregnancy ends. KORE dedicated state resources for prevention, increase access to MAT, increase recovery support services designed to improve treatment, increase access to naloxone, and enhance statewide coordination and evaluation of health care strategies. Maryland's Health Choice 1115 Demonstration expanded eligibility and services for PPW with SUD that includes an Evidence Based Home Visiting pilot program for high risk pregnant women and children up to two years for 60 days after the pregnancy ends. New Mexico's 1115 Demonstration Waiver for Centennial Care 2.0 piloted the Nurse Family Partnership (NFP) and the Parent as Teachers (PAT) program to benefit pregnant and parenting women with OUD. NFP is a national program designed to reinforce maternal behaviors that encourage positive parent child relationship until the child reaches two. PAT provides parent with child development knowledge and parenting support until the child is five. Finally, Virginia's Innovative, Focused and Scalable Delivery System Transformation 1115 waiver covers cases management services for high risk pregnant women and children up to age two, including pregnant women with SUD. This includes expanded prenatal care services, patient education, nutritional assessment counseling and follow-up, homemaker services and blood glucose meters for 60 days after the pregnancy ends.
In addition to 1115 waivers, a few states have expanded Medicaid eligibility and services covered by Medicaid. In Illinois, the state leveraged the Illinois Opioid Action Plan to increase access to MAT for PPW and outlined Medicaid eligibility under Managed Care Organizations for treatment of OUD including PPW for 60 days after the pregnancy ends. This included expanding Medicaid eligibility and services covered by Medicaid as well as providing comprehensive resources through the Opioid Use Treatment Resource Manual. Illinois leveraged the Illinois' State Targeted Response to the Opioid Crisis Grant (STR Grant) to fund prevention, treatment, and recovery programs across the state. In Wisconsin, the State Plan under Title XIX of the Social Security Act expanded case management services that includes a face-to-face or telephone contact every 30 days if the child is aged six months or less and contact with the recipient every 60 days if the child is aged 12 months or less. The covered activities include periodic reassessments and time spent on recordkeeping, which includes updating the care plan, documenting patient contacts, preparing and responding to correspondence to the patients contact, and documenting the patient's activities in relation to the care plan.
4.2. Eligibility Rules and Requirements Across States
Eligibility requirements for standalone programs treating pregnant and parenting women with OUD vary across programs. Some requirements, such as a proven record of sobriety prior to entering the program and limitations placed on the age of children who can accompany pregnant and parenting women in residential treatment could potentially create a barrier to family-centered care.
Mechanisms used to fund statewide treatment initiatives are accompanied by program eligibility requirements that dictate the type of services provided or duration of care. Statewide requirements can be both facilitators and barriers to treatment. Some states require that providers report when substance use by pregnant women is confirmed or suspected. In a subset of these states substance use during pregnancy is legally defined as child abuse or can be used as grounds for civil commitment. At the same time, many states require general programs to give priority access to pregnant and parenting women and protect women from discrimination in publicly funded programs. Under the rules of SAMHSA's Substance Abuse Block Grant, every state has to provide priority access to treatment for pregnant women. A review of state policies for selected states is provided in Exhibit 2.
| EXHIBIT 2. State Policies Regarding Reporting and Treatment of PPW with OUD Across Selected States | |||||||
|---|---|---|---|---|---|---|---|
| Require Reporting of Suspected Drug Use |
Require Providers to Test for Drugs if Use is Suspected |
Drug Use During Pregnancy is Considered Child Abuse |
Drug Use During Pregnancy is Grounds for Civil Commitment |
Priority Access to Treatment Given to Women |
Protections Against Discrimination for Women Seeking Treatment |
Targeted Program and Other Policies for PPW with SUD |
|
| California | X | X | |||||
| Delaware | X | ||||||
| Florida | X | X | X | ||||
| Illinois | X | X | X | X | X | ||
| Kentucky | X | X | X | X | X | X | |
| Maine | X | X | |||||
| Maryland | X | ||||||
| Massachusetts | X | ||||||
| Mississippi | X | ||||||
| Montana | X | ||||||
| New Hampshire | X | ||||||
| New Mexico | X | ||||||
| North Carolina | X | ||||||
| Ohio | X | X | X | X | X | ||
| Pennsylvania | X | X | |||||
| Rhode Island | X | X | X | ||||
| Texas | X | ||||||
| Utah | X | X | X | ||||
| Vermont | |||||||
| Virginia | X | X | X | ||||
| Wisconsin | X | X | X | X | X* | ||
| * Information retrieved from Guttmacher Institute in July 2018, https://www.guttmacher.org/state-policy/explore/substance-use-during-pregnancy. | |||||||
4.3. Care Coordination
Care coordination is a key component of family-centered MAT for pregnant and parenting women. High-quality family-centered care coordination incorporates clinical care and coordination with non-clinical resources as well as other state agencies and local resources. Care coordination varies widely by state and program but most programs treating pregnant and parenting women with OUD incorporate some level of care coordination.
Treatment programs for pregnant and parenting women offer an array of clinical and non-clinical services to support recovery. For example, New Expectations in Delaware provides MAT, clinical counseling, peer specialists, and recovery coaches. The Moms in Recovery (MIR) Program in New Hampshire offers a range of coordination services such as help accessing housing, transportation, insurance and employment support, in addition to coordinating physical health, mental health and OUD treatment.
Statewide initiatives typically include coordination of clinical and non-clinical services. For example, the Birth to 3 Program in Wisconsin, a State Plan Amendment, provides case management to PPW. A requirement of this initiative is that the case manager identify and schedule at least the initial appointment for all clinical and non-clinical services for participating PPW.
4.4. Statewide Initiatives for Capacity Building
The North Carolina Pregnancy and Opioid Exposure Project is an umbrella under which information, resources and technical assistance are disseminated regarding the subject of pregnancy and opioid exposure. The project is hosted by the University of North Carolina (UNC) School of Social Work and is funded by federal Substance Abuse Prevention and Treatment Block Grant funds. The State of Illinois supported a collaborative effort to develop a resource, the Opioid Use Treatment Resource manual, to create awareness about available treatment resources for pregnant Illinois women who are insured by Medicaid and to illuminate geographical areas with gaps in services. In addition, the Women's Plan and Practitioner's Toolkit was created by the Women's Committee of the Illinois Advisory Council on Alcoholism and Other Drug Dependency for the Illinois Department of Human Services/Division of Alcoholism and Drug Abuse. The toolkit includes trainings and resources to create innovative and best practices programming to ensure appropriate care to women and their families. It also builds collaborative teams between child welfare, public health, substance abuse and mental health community providers and medical professionals to address policy and practice to address the needs of pregnant women with OUD.
4.5. Partnerships
States are engaging in a number of different partnerships to support treatment for pregnant and parenting women with OUD. State agency and university partnerships support multiple educational, funding and data collection initiatives. The Massachusetts Technical Assistance Partnership for Prevention (MassTAPP) supports communities across the state in addressing substance abuse prevention and treatment. Funded by the state and SAMHSA, the partnership offers multiple training and technical assistance opportunities and supports capacity building throughout the state for expansion of SUD services, including services to pregnant and parenting women.
Many states are building upon the federal requirements of the Comprehensive Addiction and Recovery Act of 2016 to strengthen data capture efforts around identification and treatment of infants with NAS and their mothers and engaging in collaborative statewide measurement and evaluation efforts. Many of these have developed task forces, committees, projects, and toolkits to conduct data collection activities for statewide measurement and evaluation efforts. Exhibit 3 demonstrates states with task forces, committees, projects and toolkits for these purposes.
| EXHIBIT 3. Statewide Partnerships for PPW with OUD | ||
|---|---|---|
| State | Initiative | Objective of Initiative |
| Illinois | NAS Advisory Committee | NAS Advisory Committee assists the Department of Public Health with developing appropriate and uniform definitions, identification processes, hospital training protocols, and reporting options with respect to NAS, as well as to make recommendations on evidence-based guidelines and programs to improve pregnancy outcomes. |
| Mississippi | Governor's Opioid and Heroin Study Task Force | The Governor's Opioid and Heroin Study Task Force provides recommendations of how to best fight opioid and heroin abuse and how to prevent it in the future. Pregnant and parenting women were named as a target group for these efforts and the expansion of MAT. |
| New Hampshire | Perinatal Substance Exposure Task Force; Data Collection and Evaluation Task Force | Perinatal Substance Exposure Task Force advises the Commission on ways to lessen barriers pregnant women face when seeking quality health care, aligning state policy and activities with best medical practices for pregnant and newly parenting women and their children, and increasing public awareness about the dangers of exposure to prescription and illicit drugs, alcohol and other substances during pregnancy. Data Collection and Evaluation Task Force is working to identify the most appropriate tools for evaluating New Hampshire's alcohol and drug abuse programs. The task force is planning to publish data through an online data dashboard. |
| Rhode Island | NAS Task Force | NAS Task Force developed guidelines for maternal and neonatal management of substance exposure, neonatal withdrawal and other drug effects. The Task Force has developed a 2-year plan with work groups that focuses on: (1) peer supports for pregnant and parenting recoverees; (2) prenatal referral and linkage to care (substance use treatment, prenatal care, family support programs); and (3) hospital protocols for supporting substance exposed pregnancies at delivery. |
In addition, many states participate in the national initiative which is a quality improvement initiative for addressing maternal mortality and severe morbidity in birth centers funded by the Health Resources and Services Administration (HRSA). The Alliance for Innovation on Maternal Health (AIM) is a maternal safety bundle program that developed best practices for maternity care and is endorsed by national multidisciplinary program. These maternal safety bundles include action measures for: (1) Obstetrical Hemorrhage; (2) Severe Hypertension/Preeclampsia; (3) Prevention of Venous Thromboembolism; (4) Reduction of Low Risk Primary Cesarean Births/Support for Intended Vaginal Birth; and (5) Reduction of Peripartum Racial Disparities Postpartum care access and standards. States participating in AIM featured in the scan include New Mexico, Texas, Illinois, Massachusetts, Maryland, Ohio, New Hampshire, Vermont, and Maine.
5. FINDINGS FROM INTERVIEWS
5.1. Overview
During our key information interviews, we spoke with state officials in four states (New Hampshire, Ohio, Pennsylvania, and Texas) and with provider organizations in three of these states (New Hampshire, Ohio, and Pennsylvania). Collectively, these interviews allowed us to explore the components of family-centered treatment programs across the country, the extent to which they are available in these states, and the ways in which states are approaching program eligibility, funding, community linkages and partnerships, and common barriers to access.
Exhibit 4 summarizes key dimensions of MAT treatment programs in these four states. In the following case studies, we provide a more detailed look at the ways in which states have structured and funded their programs.
| EXHIBIT 4. Key Dimension of MAT Treatment Programs | ||||
|---|---|---|---|---|
| New Hampshire | Ohio | Pennsylvania | Texas | |
| Program | MIR | MOMS | COEs | Mommies |
| Eligibility | No state requirements for eligibility | State requires that woman must be 18 years of age or older and diagnosed with a SUD | No state requirements for eligibility | No state requirements for eligibility |
| Funding | STR funds and Delivery System Reform Incentive Payment waiver which funds intensive outpatient and case management services | MOMs initially funded with $4.2 million from the Governor; presently financed with STR funds | STR funds and earmarked state dollars for COEs | STR funds and general revenue funds |
| Family-centered Services | MAT, SUD treatment and counseling, recovery support services, child care, parenting classes, and case management | MAT, prenatal and postnatal care, SUD treatment and counseling, child care, and recovery support services | MAT, prenatal and postnatal care, SUD treatment and counseling, child care, family planning services, and parenting classes | MAT, prenatal and postnatal care, SUD treatment and counseling, child care, parenting classes, life skills education, case management |
| Community Linkages | Varies by site but generally linkages to child care, income support, housing, job training, and transportation. | Varies by site but generally linkages to transportation, child care, and housing. | Varies by site but COE's operate under a "hub and spoke" model where provider connects women to a range of services including housing, job training, child care, and transportation. | Case management is offered to facilitate access to medical care and connect pregnant women with needed resources in the community. |
| Partnerships | State is partnering with the Department of Children Youth and Families to assist children whose parents are struggling with SUD. The state has also created a Perinatal Substance Exposure Task to recommend strategies for aiding pregnant and parenting women with SUDs. | Statewide steering committee comprised of staff from various state agencies, MOMS providers, the Ohio College of Medicine, and managed care organizations oversees the MOMS initiative. State is also training MOMs providers to build relationships with local child welfare agencies. | The state is partnering with the March of Dimes to develop perinatal collaborative focused on pregnant women with OUD and NAS. | The Mommies program involves collaboration between the Methadone Treatment Center, Texas DSHS, and University Health System. The state is partnering with the state child welfare agency to develop a Mommies Education program. |
5.2. New Hampshire Case Study
5.2.1. Overview of State Initiatives
Dartmouth-Hitchcock's MIR program is a leader in the fight against OUD among pregnant women in New Hampshire. The MIR program was created in 2013 after a group of hospital obstetricians and gynecologists (OB-GYNs) observed an increase in the number of pregnant mothers with SUD missing their prenatal visits at the Dartmouth clinic. The program now offers an intensive outpatient treatment program, which includes MAT and a range of other services, to pregnant women with histories of opioid abuse. Funded through a 21st Century Cures grant of $2.7 million, MIR is currently being expanded to seven additional maternity care practices throughout the state.
The Bureau of Drug and Alcohol Services has also created a best practice guide for delivering community-based MAT services for OUDs. Intended to increase access to MAT services statewide, the guide outlines requirements for implementing a MAT program in a primary care clinic, behavioral health setting, or a free-standing MAT or methadone clinic. The guide does not specifically discuss considerations pertaining to pregnant women.[9]
5.2.2. Family-Centered Services and Care Coordination
MIR sites offer MAT, group and individual SUD treatment and counseling, recovery coaching, parenting classes, and case management services. Child care is made available to all women during their visits. Case managers perform a psychosocial assessment and use a social determinants of health screener to help link women to an array of community services including income support, housing, job training, and transportation. All OB-GYNs receive training in trauma-informed care.
The Dartmouth-Hitchcock location also has a midwife located on site as well as primary care, obstetrics, and mental health clinicians. A pediatrician visits the clinic twice a month. Although other MIR sites are encouraged to replicate the Dartmouth-Hitchcock model, the state allows flexibility in implementation to accommodate variations in providers and regions. Family members can attend treatment meetings when they are supportive. Dartmouth-Hitchcock originally offered individual sessions for fathers at one time, but they discontinued this service because many relationships were abusive. Now, they refer male partners to the general SUD treatment program at the hospital.
The Dartmouth-Hitchcock MIR program has also evolved to provide on-going support to women for many months and sometimes years after delivery. This extension of services was aided in part by New Hampshire's decision to expand Medicaid in 2014 which allows more pregnant women to retain their Medicaid coverage after delivery.
5.2.3. Partnerships
Modelled after Kentucky's Sobriety Treatment and Recovery Team program, New Hampshire is partnering with the Department of Children, Youth and Families to help children involved with the child welfare system whose parents are struggling with SUD. Titled Strengths to Succeed, the program would provide fast-track access to SUD treatment services for parents as well as counseling and services for the children. Child welfare workers would partner with family mentors who have achieved sobriety and have experience with the child welfare system to assist families.
New Hampshire has also created a Perinatal Substance Exposure Task Force, whose mission is to educate and inform the Governor's Commission on Alcohol and Drug Abuse, Prevention, Treatment and Recovery on pertinent issues related to pregnant and parenting women with SUDs. The Task Force, which was created in 2015, is currently working in collaboration with the Division of Public Health Services and the Division of Children, Youth and Families on developing a Safe Plan of Care for women impacted by substance use. The Task Force is planning a summit scheduled for January 2019 to discuss optimizing care for mothers and babies affected by SUD.
5.3. Ohio Case Study
5.3.1. Overview of State Initiatives
In response, the state created the Maternal Opiate Medical Supports (MOMS) initiative which officially launched as a pilot in mid-2014. The MOMS initiative provides treatment to pregnant mothers with opiate issues during and after pregnancy through a Maternal Care Home (MCH) model of care. MOMS began as a partnership between the Ohio Governor's Office of Health Transformation, the Department of Mental Health and Addiction Services, and the state's Medicaid agency. Currently there are nine provider sites implementing the MOMS model and the state expects to add three more sites by the end of 2018. All 12 sites are public behavioral health providers or federally licensed opioid treatment program (OTP) providers.
|
As compared to a Medicaid comparison group:
Rick Massatti, Ohio Department of Mental Health and Addiction, Improving Maternal-Infant Outcomes. Presentation for Department of Health and Human Services (April 2018). |
The state's Perinatal Quality Collaborative, a Medicaid-funded consortium founded in 2007, launched MOMS+ in 2018 to train individual obstetricians and maternity care providers on how to recognize and treat OUD in pregnant women. The goal of MOMS+ is to reach those pregnant women who do not have access to a local behavioral health provider. Through a mentor-partner model, the program aims to expand the capacity of maternity care providers to treat pregnant women by providing or arranging for MAT, behavioral health counseling, and other social services. Full implementation of MOMS+ is expected to be completed by the end of 2018. The Collaborative has also developed a NAS protocol to assist states and providers reduce hospital length of stay among newborns with NAS.
Initially funded via a $4.2 million grant from the state, Ohio is applying some of its Phase 1 and Phase 2 grant funding from the Opioid STR Grants initiative to sustain the program. The state intends to continue financing its MOMS initiative in future years with Medicaid funding.
5.3.2. Family-Centered Services and Care Coordination
Each MOMS' provider varies slightly in types of services they offer but they are all required to directly offer or provide access to the following services: MAT, prenatal and postnatal care, SUD treatment and counseling, housing, and recovery support services.[10] The model emphasizes team-based care and care management for moms and babies. Some offer inpatient residential treatment whereas others provide outpatient services only. Targeted programming for dads is not a key element of MOMS at present, although the state intends to emphasize this with its MOMS expansion. MOMS providers are also strongly encouraged to co-locate clinical providers such as obstetricians and pediatricians on-site throughout the week.
First Step Home is an addiction recovery center for women in Greater Cincinnati, funded through the MOMs program, which allows women to live with their children up to age 12, as they recover from their SUD. The Center provides individual and family counseling, mental health services, MAT, residential treatment, transitional housing, parenting classes, vocational counseling, and continued outpatient treatment, case management for the newborn and coordination with pediatric and family health care. The program has found that housing is critical to ensuring stability; women have a very hard time finding safe/affordable housing in the community after residential treatment so First Step is increasing its housing options on site. Apart from the on-campus housing and residential program, First Step Home also operates The Terry Schoenling Home for Mothers and Infants, an eight-bedroom house that helps women with OUD bond with their newborns from two weeks before delivery to 30 days postpartum.
MOMS sites are required to create community linkages with non-clinical entities to help women transition back into daily life after giving birth. This includes linkages with child care providers, transportation entities, housing support organizations, employment resources, and others. The state encourages new MOMS sites to complete a "community readiness" process, which involves holding meetings with stakeholders in the community to educate them about the program, solicit their support, and build relationships.
To further incentivize care coordination and care integration for treatment of behavioral health conditions and SUD, Ohio is designing a qualified behavioral health entities (QBHE) initiative in its Medicaid program, scheduled to launch in 2019. Under the QBHE program, qualified providers may be eligible to receive an additional $200 per-member, per-month to better coordinate SUD services and deliver wrap around care (i.e., education, social services, etc.) to pregnant women and their families. MOMS providers are eligible to participate.[11]
5.3.3. Partnerships
A statewide steering committee oversees the MOMS initiative. The committee is comprised of representatives from the state Office of Health Transformation, the Department of Mental Health and Addiction, and the state Medicaid agency, as well as participating MOMS providers, evaluators from the Ohio College of Medicine, and representatives from managed care organizations.
To promote collaboration between MOMS providers and state agencies, the steering committee partnered with the state Department of Job and Family Services to help MOMS sites build relationships with their local child welfare agency. Child welfare agencies help MOMS providers understand state reporting requirements and legal mandates and MOMS providers educate local child welfare agencies about MAT and their services for pregnant and parenting women.[12] As required by the Child Abuse Prevention and Treatment Act of 2015, child welfare authorities are required to complete a plan of safe care for each infant born to a woman with a SUD. As a result of these partnerships, pregnant women are working jointly with their MOMS providers and child welfare caseworkers to develop these plans of care. Child welfare agencies can also assist in providing resources to support a women's recovery pre-delivery and post-delivery.
As mentioned above, the state Medicaid agency also created the Ohio Perinatal Quality Collaborative -- a statewide consortium consisting of perinatal clinicians, hospitals, policymakers and governmental entities which created the MOMS+ initiative in 2018.
5.4. Pennsylvania Case Study
5.4.1. Overview of State Initiatives
Centers of Excellence (COEs) began in Pennsylvania in 2016 in response to the opioid crisis. COEs act as health homes for Medicaid-insured individuals with OUD, and they provide a high level of care coordination and integration of behavioral health and primary care. Pregnant women with OUD have been identified as a priority population in this initiative. COEs operate under a "hub and spoke" model, in which the designated center serves as a health home and connects individuals to needed care throughout the community, through partnership with hospitals, providers, correctional facilities, law enforcement, courts, emergency medical services, and more. There are currently 45 COEs across the state, 25 of which are behavioral health entities and 20 of which are physical health entities. These COEs are located in both urban and rural areas.
|
Funding
|
One COE, Magee-Women's Hospital of the University of Pittsburgh Medical Center (UPMC), has operated a Pregnancy Recovery Center for pregnant women with OUD since 2014. The Center provides office-based buprenorphine treatment, behavioral health counseling, social services, and prenatal care.
The state is also funding large health systems to be care coordination "super hubs," described by one state official as "COEs on steroids." There are currently nine super hubs across the state that work with communities to provide intensive care coordination through a team of care management staff to ensure that everyone with OUD -- including pregnant women -- is connected to the appropriate resources and care. Super hubs will also provide training to other COEs. Pennsylvania has also contractual requirements with their managed care plans to develop health homes for pregnant women within high-volume OB-GYN health systems. These health homes are expected to have contracts in place to support and supplement care management activities for pregnant women.
Pennsylvania expanded Medicaid eligibility under the Patient Protection and Affordable Care Act (ACA), which led to approximately 710,000 adults who were newly eligible for Medicaid coverage. The state has a behavioral health "carve out," and both physical and behavioral health and overseen by managed care organizations.
5.4.2. Family-Centered Services and Care Coordination
COEs, super hubs, and managed care health homes are all encouraged to look beyond medical aspects of treatment and care management and focus on social determinants of health like housing, domestic violence, food insecurity, and reestablishing family relationships. Additionally, they are encouraged to take a trauma-informed and trauma-responsive approach to treatment that acknowledges and addresses the underlying trauma that exists for many individuals with OUD. The Pregnancy Recovery Center at Magee-Women's Hospital -- which characterizes itself at women-centered, rather than family-centered -- provides child care, prenatal and postpartum care, pregnancy-specific dosing, housing and transportation assistance, breastfeeding education and support, family planning counseling, sexually transmitted infection screening, parenting skills training, and individual and group counseling.
Some COEs take a broad approach to treatment, with increasing engagement of family members such as the father, grandparents, and expended family. One state official noted that Medicaid expansion has allowed many more males to be covered in Pennsylvania, and COEs want to engage these individuals in a family-centered treatment model.
Care coordination is integral to the COE "hub and spoke" model of care. The care management team oversees comprehensive, wraparound care for individuals in their care and makes referrals to community partners when for needs that cannot be met internally (e.g., housing, job training, and -- for that that do not provide MAT themselves -- community-based MAT providers). Some women seek care at a COE that is far from their home, due to a lack of intensive resources closer to them, and the COE can also help them find counseling in their community.
5.4.3. Partnerships
Pennsylvania reports robust partnerships throughout the state with few barriers to collaboration. Explained one state official, "People are very receptive [to collaboration]. This is a crisis, with 13-14 Pennsylvanians dying every day." The state is currently working with the March of Dimes and another non-profit organization in the state to develop a statewide and regional perinatal collaborative focused on both pregnant women with OUD and NAS babies. The collaborative -- which is still in development and aims to operationalize in the last quarter of 2018 -- will bring together partners including the Department of Drug and Alcohol Programs, Department of Health, Department of Health and Human Services, and various provider stakeholders. Another partnership is supported through recent legislation which mandated the creation of a statewide maternal mortality review, based off the Philadelphia review process, which will involve multiple state agencies and be overseen by the Department of Health. Also, non-state partnerships in the state include faith-based collaboratives that bring together community partners to support individuals with OUD, though these are not specific to pregnant women.
5.5. Texas Case Study
5.5.1. Overview of State Initiatives
In 2007, Project Cariño launched in San Antonio through a $2.5 million PPW grant to the Center for Health Care Services (CHCS), the local mental health authority. At the time, one-third of all cases of NAS in Texas were concentrated in Bexar County (where San Antonio is located). The program provided comprehensive substance use and mental health services (offered by CHCS) with prenatal and neonatal care through a local hospital system. The program sought to improve birth outcomes for babies born to mothers with SUD, provide prenatal education and care, and shift provider attitudes and behaviors around this population of pregnant women. Together, these efforts contributed towards a reduction in length of neonatal intensive care unit (NICU) stays for NAS babies by 33 percent.[13]
|
Since the Mommies Program began in San Antonio, Texas, average NICU length of stay for NAS babies has decreased by 33%. |
Inspired by these positive results, the Texas Department of State Health Services (DSHS) expanded the program to other hospitals statewide in 2013 and changed the named to the Mommies Program. This name was described by state officials as a "stigma reducing term" that indicated to providers that a pregnant woman with SUD was "just one of the other mommies." The program provides intensive outpatient treatment -- including MAT -- for pregnant and parenting women with SUD.
In addition to the Mommies Program, Texas has a continuum of treatment for SUD services that ranges from prevention to intervention to clinical. Texas is participating in the national HRSA AIM program and plans to pilot the opioid bundle in nine hospitals, seven of which are original Mommies program. An implementation plan is currently in development.
Texas did not expand Medicaid eligibility under the ACA. Medicaid covers MAT, but pregnancy-related Medicaid coverage is typically terminated six weeks postpartum. Some general revenue state funding is available through NAS-opioid treatment service providers to provide women with MAT services after they have exhausted their pregnancy-related Medicaid through 18 months postpartum, with the goal of avoiding treatment disruption.
5.5.2. Family-Centered Services and Care Coordination
Mommies programs coordinate wraparound services for pregnant and parenting women with any type of SUD, and provide MAT during pregnancy, a postpartum recovery program, and 13-weeks of parenting and life skills education. An individualized treatment plan is developed for all participants and may include substance abuse counseling, crisis intervention, case management, individual therapy, family therapy, and group therapy. All women in the program with OUD enter into MAT. Programs employ evidence-based models including the Trauma, Recovery, and Empowerment Model, which focuses on recovery from trauma and abuse through gender-specific treatment, and Seeking Safety, which addresses trauma and addiction. A patient navigator or recovery coach (both terms are used) -- a degreed professional with lived SUD experience -- is accessible 24 hours a day via cell phone and acts as a coach, role model, and advocate as participants interface with other agencies. They also assist with coordinating educational sessions. Although Mommies is women-specific, Texas also has a Parenting Awareness and Drug Risk Education program for expectant and parenting fathers.
|
Funding The statewide Mommies Program is funded primarily through general revenue in the annual budget. Most recently, it was allocated $11.2 million over a two-year period. Other funding for SUD treatment in the state comes from federal grant funding (21st Century Cures Act, STR to the Opioid Crisis Grants, and SOR Grants), block grant funding, state general revenue dollars, and Medicaid reimbursement for certain clinical services. Prevention and intervention services are typically non-billable and funded through program contracts. |
Mommies programs are contractually obligated to provide therapeutic and clinical services, but the nature of service provision varies. Some sites provide all services on-site, including clinical services like vision and dental, while others partner with providers in the community.
5.5.3. Partnerships
The Mommies program involves public-private collaboration between Mommies Program is a collaboration between the Methadone Treatment Center, Texas DSHS, and University Health System. The program also partners with a variety of service-providing agencies that working with participating women, such as the Adult Probation Department.
Additionally, the Texas DSHS has partnered with the state child welfare agency to develop a Mommies Education program. This program began due to child welfare desire to be involved with pregnant women with OUD before the child is born and provide a complete treatment plan around prenatal care, education, and other aspects related to the care of the child. Mommies Education provides prenatal education targeted to this population of pregnant women and covers topics that may not be discussed in traditional parenting classes, such as pain management while on methadone and NICU visitation.
6. CHALLENGES AND OPPORTUNITIES RELATED TO TREATMENT
6.1. Insurance Coverage
6.1.1. Challenges
Respondents from the interviewed states discussed challenges faced by women insured by Medicaid and by private plans. One state official noted substantial variation in covered treatment services among private plans in the state; for example, one plan will reimburse members for residential treatment services but not higher-level specialty services for pregnant and parenting women. This lack of consistency among plans presents challenges for this group of women.
Most of the barriers discussed were on the Medicaid side, however. In states that did not expand Medicaid eligibility under the ACA, many low-income women are uninsured until they become pregnant, obtain pregnancy-related Medicaid coverage during pregnancy and delivery, and then lose this coverage several weeks postpartum. At this point, as one state official explained, "Babies have coverage, but where does the mother go for treatment?" Women may initiate MAT upon gaining temporary Medicaid coverage and then discontinue when they lose coverage postpartum. This abrupt discontinuation of treatment during a vulnerable period of time can prove dangerous and lead to relapse. In non-expansion states, some women are eligible for Medicaid coverage due to their status as a parent to dependent children. Federal officials discussed that in these states, a woman can lose coverage if she enters residential treatment without her children, as she may be required to give up her caregiver status.
Even women who are insured by Medicaid may face barriers to accessing treatment, due to limited scope of coverage. Methadone is not covered under every state program, and one provider explained that in recent years, their state government limited their ability to bill Medicaid for case management in certain outpatient treatment settings. Other non-reimbursable services mentioned across states include professionals such as peer recovery coaches, care managers, lactation consultants, and child life specialists.[14]
In addition, some providers do not accept any insurance. One researcher discussed a recent survey of treatment providers (specifically, opioid agonist providers, OTPs, and outpatient buprenorphine providers) in four states in Appalachia, which found that just over half of these providers accepted any form of insurance and some were unwilling to accept pregnant patients, even when they were accepting new patients more generally.
6.1.2. Opportunities
Interviews with stakeholders in states that expanded Medicaid eligibility highlighted the key role that expansion can play in increasing access to family-centered treatment. In these states, nearly all low-income women are eligible for Medicaid coverage, and -- unlike in non-expansion states -- this coverage does not end in the immediate postpartum period. Low-income men also have substantially more pathways to Medicaid coverage in these states, which presents an opportunity to engaging partners and co-parents in treatment.
Some states have also utilized Section 1115 Medicaid Demonstration Waivers to expand access to treatment for Medicaid beneficiaries. Kentucky, Maryland, and New Mexico were identified as such states; for example, Maryland implemented an 1115 Demonstration to expand eligibility and services for PPW with SUD.
Additionally, some respondents indicated a preference towards the adoption of more non-fee-for-service payment policies that support incentivizing providers to work in systems such as Accountable Care Organizations or Accountable Health Communities, which allow providers greater flexibility in how they organize and deliver treatment.
6.2. Funding Constraints
6.2.1. Challenges
Insurance coverage is a critical piece of the funding landscape for family-centered OUD treatment, and Medicaid expansion provides a significant and effective opportunity to increase access to this coverage. However, as noted previously, there are a number of non-clinical services -- ranging from care coordination to child care -- that are considered key to family-centered treatment but are not typically reimbursable under Medicaid. Most respondents -- researchers, providers, and government officials -- named funding as a key barrier to expanding access to family-centered MAT programs. Explained one federal official, "I think it's a financing issue more than a desire to not [provide this care]." Funding can prove challenging in a variety of ways. Some respondents, particularly providers, noted that insufficient funding overall has required them to reduce their length of inpatient stay; one organization has reduced their length of stay by 25 percent based on a lack of increase in block grant funding, rather than on best practices or evidence. This provider explained that reduced length of stay is problematic because longer time in treatment is associated with better outcomes for women and their children. These reductions started over the last 2-3 years as the cost of business increased and block grant dollars remained stable. Insufficient funding has also presented challenges for staff recruitment, as programs have a cap on what they can pay employees.
Finally, while many respondents acknowledged the surge of funding currently available to address the opioid crisis, there were concerns about sustainability and flexibility of this funding. One provider explained that "programs and providers are scared to death" because they do not see a plan for sustained funds after 2-3 years, leading to reluctance to expand beds and services; others felt that these feats were not merited and that funding did allow for sustainable investments in treatment programs. Some stakeholders also cited challenges around funding specific to opioid use, because this targeted funding does not allow them the flexibility to treat other SUDs more generally. Two states mentioned methamphetamine use as a problem as severe -- or more severe -- as opioid use in their state, but without the same level of targeted funding.
6.2.2. Opportunities
The states interviewed and included in the program scan cited a wide-range of funding sources used to implement, sustain, and expand access to OUD treatment models, indicative of the profusion of federal funding that has been made available in response to the opioid crises. State Targeted Response to the Opioid Crisis Grants (Opioid STR) individual grant awards have been utilized by many states, including Delaware, Florida, Kentucky, Maine, Mississippi, Montana, New Hampshire, Texas, Utah, and Wisconsin. The Residential Treatment for Pregnant and Postpartum Women grant program was another commonly used sources of funding for states in this review.
Other sources of funding include State Opioid Response (SOR) grant funding, block grants, state funds, CDC funding, and additional flexibilities in Medicaid funding through Section 1115 Demonstration waivers or State Plan Amendments.
6.3. Workforce Capacity Shortages
6.3.1. Challenges
Respondents from all states mentioned experiencing shortages across several types of addiction professionals -- clinical social workers, licensed alcohol and drug counselors, and psychiatrists. Finding enough addiction professionals was identified as particularly problematic in rural areas throughout Ohio, Pennsylvania, and New Hampshire. Shortages were attributed to insufficient training in addiction medicine for clinical and non-clinical professionals (e.g., child life specialist, peer providers, care coordinators) as well as a limited pool of applicants. Obstetricians, pediatricians, and family medicine doctors would all benefit from additional education around treating pregnant women and other adults with SUDs, noted one stakeholder. Respondents also noted that many addiction providers cannot afford to pay health care professionals high enough salaries to attract them for permanent positions. Often times they will take a position with the provider for one year and then move on to higher paying positions.
6.3.2. Opportunities
To address workforce challenges, states identified a few solutions. For example, Ohio is using funds from STR grants (authorized by the 21st Century Cures Act) to increase the number of waivered physicians across the state that can deliver MAT. The Ohio Medicaid Department is also working with managed care organizations to develop criteria for "gold carding" physicians who may need to treat patients with OUD. Physicians who receive a "gold card" would be exempt from meeting plans' prior authorization requirements to deliver MAT. To aid in recruitment and retention efforts, Ohio has also created loan forgiveness programs for health care professionals in previous years.
In New Hampshire, state officials have created a workforce development task force to identify strategies for recruiting and training qualified professionals to treat individuals with a SUD.
6.4. Limited Access to Safe and Affordable Housing
6.4.1. Challenges
Depending on the state and county where they reside, pregnant women have varying levels of access to residential treatment. Additionally, not all residential programs allow children to stay with moms during their inpatient stay making it difficult for these moms to care and bond with their children throughout treatment. As a result, many women elect to receive outpatient services and have to rely on friends, family, and sometimes partners to provide them with housing during treatment. In some cases, these family members and/or partners may be abusive or using substances themselves impeding a woman's recovery.
Respondents also expressed frustration with the lack of affordable housing available in their communities. This includes affordable housing for moms to reside in during treatment and after treatment. Some respondents noted that there simply was not enough public funding available to subsidize housing options. Other barriers to finding housing identified by stakeholders included stigma among recovery housing providers against individuals on MAT and an unwillingness on the part of landlords to rent to individuals with a history of substance use.
6.4.2. Opportunities
Some providers are actively involved in working with federal and state regulators to either purchase or rent apartment buildings for women to stay in during and after recovery. For example, one provider in Ohio described working with the U.S. Department of Housing and Urban Development to purchase a 23-unit apartment building to support women and their families throughout the recovery process. After limited success securing affordable housing in the community, this provider opted to increase its recovery housing options on site.
6.5. Provider Reluctance to use MAT
6.5.1. Challenges
Despite recent studies indicating that MAT is the preferred form of treatment for pregnant women, some stakeholders reported that provider resistance to treating patients with an OUD does inhibit state efforts to expand access. According to one recent study published in the Annals of Family Medicine, only 46.6 percent of United States counties (1,465 of 3,143) had a waivered physician who could prescribe buprenorphine. Of the counties that had no physicians who could prescribe buprenorphine, 82.1 percent were in rural areas.[15] One state official also noted that even after receiving a waiver, some physicians remain reluctant to use it. Stakeholders attribute this resistance to a number of factors including a lack of education and awareness about the efficacy of MAT, discomfort treating patients with an addiction, or a longstanding belief among health care professionals that you should not treat a SUD with a medication.
6.5.2. Opportunities
One state official reported having some success in overcoming some of this resistance by recruiting mentors to work with newly waivered physicians to increase their comfort level in managing patients.
7. ADDITIONAL FINDINGS
As this review of how states are incorporating family-centered treatment principles into MAT services for PPW with OUD indicates, state programs and policies regarding family-centered care are wide-ranging and evolving. Since the opioid crisis continues to demonstrate adverse outcomes, states will need to continue to support efforts to treat women and their families. The incorporation of family-centered components into treatment can assist women in maintaining their role of caregiver as they go through their recovery process. We offer recommendations for areas of focus and next steps for funding and policy development.
The concepts of family-centered treatment may improve access to MAT to help support recovery from OUD. When thinking about expanding family-centered treatment programs for women with SUD, it is important to consider the services and supports that are needed before, during, and after delivery to ensure that women make a full recovery. Many states appear to focus treatment resources and training efforts on women who are pregnant; however, there is a need to ensure that services and supports continue for several months after delivery to ensure adequate support for recovery (Gopman, 2014).
The concept of family should be considered in a broad sense and incorporation of treatment and programming for fathers and other key family members should be considered. While pediatric care for infants and older children is incorporated in more comprehensive treatment models, none of the programs we reviewed included specialty mental health services and early intervention for children. In addition, few state initiatives and very few programs included the women's partner as an essential component of treatment. While inclusion of partners in treatment programs can be complex due to the limitations and requirements of funding streams and the high rate of intimate partner violence and SUD among partners of PPW with OUD, efforts should be made to seek flexible funding streams and to develop treatment program models that support meaningful inclusion of partners. As stated best by an interviewee, "Once programs start engaging fathers, they have better outcomes for the whole family".
States could benefit from receiving and developing more flexible funding streams which could support payment for services for different SUDs, different service configurations and the development of alternative payment models. Some interviewees noted they would benefit from state and federal funding opportunities that were not diagnosis-specific. For example, New Hampshire and Texas are seeing a rise in methamphetamine use among pregnant women. However, the states currently do not have the resources to address this. Allowing flexibility in funding would allow states and programs to change course and address addiction issues as they are identified. Providers would also like to see more sustainable sources of funding that are not time-limited. Some perceive the drug of choice may change (i.e., the opioid crisis may wane), but that there will still be pregnant women who continue to face addiction.
The presence of flexible funding streams that provide reimbursement for case management, peer recovery coaches, and other currently non-reimbursable services and supports is key to supporting recovery. One strategy could include incentivizing the development of alternative payment models and systems of care which would allow providers the flexibility they need to create more targeted programs. For example, provision of a case rate or episode of care payment for PPW with OUD could allow providers to tailor treatment to the specific clinical and non-community-based recovery needs of the woman and increase chances of success.
Additional research would be helpful in promoting family-centered treatment. For example, research identifying effective integration models would be beneficial. States and providers could benefit from learning about how best to integrate primary care and OUD treatment for pregnant and parenting women. Research identifying treatment models that improve outcomes for women, partners and children could help advance the implementation of family-centered treatment models would also be useful.
As evidenced through this program scan and key informant interviews, several states are incorporating family-centered treatment principles into MAT services. States are leveraging several federal funding sources, state and community partnerships and state and federal policies to support evidence-based services for pregnant women and their families though barriers to comprehensive care remain.
REFERENCES
AAP Committee on Substance Use and Prevention. (2016). Medication assisted treatment of adolescents with opioid use disorders. Pediatrics, 138(3).
American Congress of Obstetricians and Gynecologists. (2012). Opioid abuse, dependence, and addiction in pregnancy. Committee Opinion No. 524. Obstetrics & Gynecology, 119(5): 1070-1076. From https://www.ncbi.nlm.nih.gov/pubmed/22525931.
American Society of Addiction Medicine. (2015). The ASAM national practice guideline for the use of medications in the treatment of addiction involving opioid use. Chevy Chase, MD: Author. From https://www.asam.org/docs/default-source/practice-support/guidelines-and-consensus-docs/asam-national-practice-guideline-supplement.pdf?sfvrsn=24.
Bagley, S.M., Wachman, E.M., Holland, E., & Brogly, S.B. (2014). Review of the assessment and management of neonatal abstinence syndrome. Addiction Science & Clinical Practice, 9(19).
Casper, T., & Arbour, M. (2014). Evidence-based nurse-driven interventions for the care of newborns with neonatal abstinence syndrome. Advances in Neonatal Care, 14(6).
Center for Behavioral Health Statistics and Quality. (2015). Behavioral health trends in the United States: Results from the 2014 National Survey on Drug Use and Health (HHS Publication No. SMA 15-4927, NSDUH Series H-50. Retrieved from http://www.samhsa.gov/data/.
Children and Families Futures. (2015). Guidance to states: Recommendations for developing family drug court guidelines. Prepared for the Office of Juvenile Justice and Delinquency Prevention (OJJDP) Office of Justice Programs. Retrieved from: http://www.cffutures.org/files/publications/FDC-Guidelines.pdf.
Dashe J.S., Jackson G.L., Olscher D.A., Zane E.H., & Wendel G.D. Jr. (1998). Opioid detoxification in pregnancy. Obstetric Gynecology, 92: 854-8.
Dennis, K., Young, N.K., & Gardner, S.G.(2008) Funding family-centered treatment for women with substance use disorders. Irvine, CA: Children and Family Futures, Inc.
Family Strengthening Policy Center. (2004). Introduction to Family Strengthening. Retrieved from: https://www.aecf.org/resources/ntroduction-to-family-strengthening/.
Feder K.A., Mojtabai R., Musci R.J., & Letourneau E.J.(2018). U.S. adults with opioid use disorder living with children: Treatment use and barriers to care. Journal of Substance Abuse Treatment, 93: 31-37.
Gopman S. (2014). Prenatal and postpartum care of women with substance use disorders. Obstetrics & Gynecology Clinics of North American, 41(2): 213-28.
Heil, S. (2011). Unintended pregnancy in ppioid-abusing women. Journal of Substance Abuse Treatment, 40(2): 199-202. Retrieved from: https://www.ncbi.nlm.nih.gov/pubmed/21036512.
Hernandez Gray, A.A. & Moore, J.E. (2017). Addressing the opioid epidemic in Medicaid managed care for women and newborns. Institute for Medicaid Innovation.
Jones, H.E., O'Grady, K.E., Malfi, D., & Tuten, M. (2008). Methadone maintenance vs. methadone taper during pregnancy: Maternal and neonatal outcomes. American Journal of Addictions, 17: 372-386.
Kaltenbach, K., Berghella, V., & Finnegan, L. (1998). Opioid dependence during pregnancy: Effects and management. Obstetrics & Gynecology Clinics of North America, 25(1): 139-151.
Kocherlakota, P. (2014). Neonatal abstinence syndrome. Pediatrics, 134(2): e547-61.
Lipari, R.N., & Van Horn, S.L. (2017). Children living with parents who have a substance use disorder. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration.
Mandell, K., & Werner, D. (2008). Guidance to states: Treatment standards for women with substance use disorders. National Association of State Alcohol and Drug Abuse Directors.
Martin, C.E., Longinaker, N., & Terplan, M. (2014). Recent trends in treatment admissions for prescription opioid abuse during pregnancy. Journal of Substance Abuse Treatment, 48(1), pp. 37-42.
National Center on Domestic Violence. (2017). Substance Use and Coercion: Policy Implications for Domestic Violence Victims. National Center on Domestic Violence, Trauma and Mental Health.
Office on Women's Health, (2016). White Paper: Opioid Use, Misuse, and Overdose in Women. Office on Women's Health.
Patrick S.W. (2018). Testimony before the United States Senate, U.S. Senate Committee on Health Education, Labor and Pensions.
Patrick, S.W., Schiff, D.M., AAP Committee on Substance Use and Prevention. (2017). A public health response to opioid use in pregnancy. Pediatrics, 139(3).
Patrick, S.W., Schumacher, R.E., Benneyworth, B.D., Krans, E.E., McAllister, J.M., & Davis, M.M. (2012). Neonatal abstinence syndrome and associated health care expenditures: United States, 2000-2009. JAMA. 307(18): 1934-40.
Patrick, S.W., Davis, M.M., Lehmann, C.U., & Cooper, W.O. (2015). Increasing incidence and geographic distribution of neonatal abstinence syndrome: United States 2009 to 2012. Journal of Perinatology, 35(8): 650-655.
Stone, A.L., Becker, L.G., Huber, A.M., & Catalano, R.F. (2012). Review of risk and protective factors of substance use and problem use in emerging adulthood. Addictive Behaviors, 37(7): 747-775.
Substance Abuse and Mental Health Services Administration. (2007). Family-Centered Treatment for Women with Substance Use Disorders -- History, Key Elements and Challenges. Retrieved from: https://www.samhsa.gov/sites/default/files/family_treatment_paper508v.pdf.
Substance Abuse and Mental Health Services Administration. (2016). A Collaborative Approach to the Treatment of Pregnant Women with Opioid Use Disorders. HHS Publication No. (SMA) 16-4978. Rockville, MD: Substance Abuse and Mental Health Services Administration.
Substance Abuse and Mental Health Services Administration. (2018) Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants. HHS Publication No. (SMA) 18-5054. Rockville, MD: Substance Abuse and Mental Health Services Administration.
Tyler, N.A., Winkelman, N.V., Kozhimannil, K.B., Davis, M.M., & Patrick, S.W. (2018). Incidence and costs of neonatal abstinence syndrome among infants with Medicaid: 2004-2014. Pediatrics, 141(4).
Werner, D., Young, N.K., Dennis, K, & Amatetti, S. (2017). Family-Centered Treatment for Women with Substance Use Disorders--History, Key Elements and Challenges. Rockville, MD: Substance Abuse and Mental Health Services Administration.
World Health Organization. (2014). Guidelines for Identification and Management of Substance Use and Substance Use Disorders in Pregnancy. Available at: http://www.who.int/substance_abuse/publications/pregnancy_guidelines/en/.
Young, N.K., Gardner, S., Otero, C., Dennis, K., Chang, R., Earle, K., & Amatetti, S. (2009). Substance-Exposed Infants: State Responses to the Problem. HHS Pub. No. (SMA) 09-4369. Rockville, MD: Substance Abuse and Mental Health Services Administration.
Zuspan, F., Gumpel, J., Mejia-Zelaya, A., Madden, J., & Davis, R. (1975). Fetal stress from methadone. American Journal Obstetrics and Gynecology. 1; 122(1): 43-6.
APPENDIX A. STATE OPIOID USE DATA
| State | Opioid Prescriptions/ 100k Persons (2015)a |
NAS Incidence Rate Averaged Over 14 Yearsb |
Rate of Women's Opioid Overdose Deaths (2016)c |
|---|---|---|---|
| California | 47.9 | 1.2 | 3.0 |
| Delaware | 80.0 | NA | 10.2 |
| Florida | 62.8 | 2.4 | 8.5 |
| Illinois | 62.8 | NA | 8.4 |
| Kentucky | 97.0 | 5.2 | 16.8 |
| Maine | 70.0 | 12.0 | 15.3 |
| Maryland | 65.6 | 7.6 | 16.1 |
| Massachusetts | 59.9 | 5.8 | 15.5 |
| Mississippi | 107.5 | 1.3 | 4.7 |
| Montana | 90.0 | NA | NA |
| New Hampshire | 66.6 | NA | 19.9 |
| New Mexico | 70.0 | 6.0 | 12.7 |
| North Carolina | 86.8 | 2.2 | 11.5 |
| Ohio | 85.8 | NA | 20.5 |
| Pennsylvania | 81.1 | NA | 10.6 |
| Rhode Island | 69.4 | 5.0 | 14.9 |
| Texas | 58.0 | NA | 3.5 |
| Utah | 73.1 | 2.0 | 13.2 |
| Vermont | 62.0 | 14.8 | 11.4 |
| Virginia | 70.0 | NA | 9.0 |
| West Virginia | 110.0 | 9.9 | 27.1 |
| Wisconsin | 69.1 | 2.4 | 11.2 |
| United States | 79.3 | NA | 8.5 |
|
|||
APPENDIX B. PROGRAM SCAN
| Background | Specialized Program | Services Included |
|---|---|---|
| California | ||
|
In 2016, there were 2,012 opioid-related overdose deaths in California--a rate of 4.9 deaths per 100,000 persons. While the overall rate has remained the same since 2012, the number of heroin and synthetic opioid-related deaths has increased from 362 to 587 and from 146 to 355 deaths, respectively. As of 2016, CA ranks 5 for opioid related deaths of women. The incidence of NAS in California has remained level from 1.2 per 1,000 births in 1999 to 1.3 per 1,000 births in 2011. |
Southern California Alcohol and Drug Programs (regional): residential treatment programs in southern California that has culturally-adapted treatment for lower income women of color. The programs include treatment with fathers and other family members as appropriate. MFI Recovery Centers (regional): residential and outpatient services that provides full continuum of care to PPW and their families. Services are also offered for a larger population. Specific locations focus on women and families, including PPW. |
For MFI Recovery Centers (regional)-Residential Programs:
MAT Outpatient Services:
|
| Delaware | ||
|
In 2016, there were 154 opioid-related overdose deaths in Delaware--a rate of 16.9 deaths per 100,000 persons and more than the national rate of 13.3 deaths per 100,000 persons. |
New Expectations (regional): residential treatment program that allows pregnant women to be redirected to a treatment facility where women and their infants can stay for up to 6 months after their child is born, in lieu of incarceration. |
Services for New Expectations include:
|
| Florida | ||
|
In 2016, there were 2,798 opioid-related overdose deaths in Florida--a rate of 14.4 deaths per 100,000 persons--compared to the national rate of 13.3 deaths per 100,000 persons. NAS incidence rates per 1,000 hospital births increased from 0.4 in 1999 to 6.3 in 2013. |
Mothers in Recovery (regional): a program created by the Memorial Healthcare System in Broward County aimed to reduce the number of babies born with NAS in response to the increase of mothers using opioids in the county. |
Services for Mothers in Recovery include:
|
| Illinois | ||
|
From 1999 to 2016, the rate increased from 3.9 to 15.3 deaths per 100,000 persons--equivalent to 483 and 1,947 annual deaths statewide. In 2015, the rate of NAS in Illinois was an estimated 2.5 NAS cases per 1,000 live births, affecting 373 newborn infants born in Illinois that year. There was a 42 percent increase in the NAS rate between 2011 and 2015 in Illinois. As of 2016, Illinois ranks 8 in opioid-related deaths for women. |
The Women's Treatment Center, Inc. and Freedom House II (regional): 2 residential treatment centers that expanded availability of treatment to PPW based on ASAM patient placement criteria. |
The Opioid Use Treatment Resource manual services include:
Integrated Prenatal Care Wraparound Services include:
|
| Kentucky | ||
|
Kentucky is among the top ten states with the highest opioid-related overdose deaths. In 2016, there were 989 opioid-related overdose deaths in Kentucky--a rate of 23.6 deaths per 100,000 persons and nearly double the national rate. The incidence of NAS in Kentucky increased from 0.4 cases per 1,000 births in 2000 to 15.0 cases per 1,000 births in 2013. As of 2016, Kentucky ranks 16 for opioid-related, |
Kentucky Moms Maternal Assistance Toward Recovery (MATR) (regional): The goal of the KY-Moms is to reduce harm to Kentucky mothers and their children from maternal substance use during and after pregnancy, while supporting Community Mental Health Centers to provide Medicaid reimbursable case management and prevention services. Supporting Mothers to Achieve Recovery Though Treatment and Supports (SMARTS) (statewide; part of Perinatal Assistance and Treatment Home (PATHways) programs) expanded treatment services and increase capacity for evidence-based treatment. The Freedom House II: Comprehensive Residential Family Treatment for Substance Abuse Recovery (CRFTSAR) (regional) project provides comprehensive, residential substance abuse treatment for PPW to decrease substance use, promote mental and physical health and financial stability, and improve family relationships, for themselves and their children. PATHways is a statewide program that integrates treatment for addiction with prenatal care, counseling and a supportive peer network. The program is based on the Centering Pregnancy model, which reduces negative outcomes and prepares women for labor, delivery and infant care through group counseling and peer support. |
For MATR:
For SMARTS:
For Freedom House II: The CRFTSAR Project:
|
| Maine | ||
|
Maine is among the top 10 states with the highest rates of opioid-related overdose deaths. In 2016, there were 301 opioid-related overdose deaths in Maine--a rate of 25.2 deaths per 100,000 persons and nearly double the national rate of 13.3 deaths per 100,000. NAS incidence rates per 1,000 hospital births, increased from 1.1 in 1999 to 30.4 in 2012. |
Bridging (statewide): Maine developed a statewide innovative model for helping families before birth, shaping NICU practices, and reducing re-hospitalizations through post-discharge support to families related to NAS care and attachment. Opioid Health Home (OHH) (statewide): offer integrated office-based MAT, opioid dependency counseling, and comprehensive care management for eligible MaineCare members and uninsured individuals with OUD. Under STR grants, OHH are required to prioritize PPW for services provided. |
Services offered under MaineCare Benefits for OHH Services:
Individual and Family Support Services include:
|
| Maryland | ||
|
Maryland is among the top 5 states with the highest rates of opioid-related overdose deaths. In 2016, nearly 30 deaths per 100,000 persons were related to opioids. The rate of NAS in Maryland rose from 6.2 in 2004 to 11.4 per 1,000 births in 2012. As of 2016, Maryland ranks 10 for opioid-related deaths of women. |
Center for a Clean Start (C4CS) (regional): outpatient services for PPW with SUD. Center for Addiction and Pregnancy (CAP) program at John Hopkins (regional): outpatient program with an available overnight housing unit for patients requiring a recovery-oriented domicile, provides a comprehensive, coordinated, and multidisciplinary approach. Behavioral Health Assessment (BHA) (statewide): state-funded residential treatment programs with preferential admissions for pregnant women. |
C4CS services:
Gender-specific services under the BHA:
CAP services:
|
| Massachusetts | ||
|
Unintentional opioid overdose has been a leading cause of death in Massachusetts since 2005, with 4½ times more people dying from overdoses than from motor vehicle accidents. An increased cost to the state health care system, associated with medical care provided to infants who experienced in-utero exposure to drugs, motivated targeted efforts to create family friendly treatment programs and resources. |
MassTAPP (statewide): supports communities across the state in addressing substance abuse prevention. Offerings:
Massachusetts Child Psychology Access Program (MCPAP) for Moms (statewide): supports primary care providers with identifying and managing their patients' mental health and substance use concerns in an environment in which child psychiatry is scarce and helps providers identify and address the mental health and substance use concerns of their pregnant and postpartum patients. Moms Do Care/Health Policy Commission (regional) is designed to expand access to MAT for pregnant women, and to enhance the services they receive. Moms Do Care utilizes a multi-pronged approach to care for PPW with OUD. Recovery, Empowerment, Social Services, Prenatal care, Education, Community and Treatment (Project RESPECT) (regional): is a high risk obstetrical and addiction recovery medical home at Boston Medical Center and Boston University School of Medicine. Project RESPECT provides services for comprehensive obstetric and SUD treatment for PPW and their infants. Journey Project: The Journey Project is an interactive web resource for pregnant and parenting women who have questions or concerns about opioid and other substance use. The Journey focuses on the stories of women with lived experience, offering information, hope, encouragement, and resources for every step of their perinatal journey. With videos, informational slideshows, resource links, and worksheets, the Journey Project seeks to empower and inform women about opioid and other substance use and pregnancy. |
MassTAPP general supports for substance abuse prevention and treatment provided to BSAS-funded programs includes:
Services specific to family friendly treatment for OUD include community events, news and resources:
MCPAP for Moms:
|
| Mississippi | ||
|
Mississippi's opioid overdose death numbers show a 57% increase from 2016 to 2017. At the end of 2016, there were 99 confirmed opioid overdose deaths reported to the Mississippi Bureau of Narcotics, by the end of 2017 there were 173 reported opioid overdose deaths. Opioid overdose deaths accounted for 67% of all overdose deaths in the state during 2017. |
Region One Mental Health (regional): comprehensive residential treatment program for addicted PPW and their children. The 4-county catchment area served by Region One includes Coahoma, Tunica, Tallahatchie, and Quitman counties. These counties are located in the Mississippi Delta, a rural, socioeconomically deprived, underserved area of Mississippi. |
Regional One Mental Health services include:
|
| Montana | ||
|
Drug overdoses are the third leading cause of injury-related death in Montana accounting for 1,334 deaths between 2003 and 2014. The rate at which Montana babies were born exposed to narcotics increased tenfold from 2000 to 2013--from 0.8 per 1,000 live births to 9 per 1,000 live births. During 2009-2013, average hospital charges for Montana newborns with NAS were $34,000 versus $6,800 for those without NAS. |
Kalispell Regional Medical Center's Birthing Center (regional): an innovative program that aimed to reinvent how its doctors care for pregnant women who use drugs. Over 3 years, the hospital developed a program that incorporated maternal care, addiction treatment and social services, so patients received the care and services they needed in 1 place. |
Center's Birthing Center Family-Centered Services for NAS:
|
| New Hampshire | ||
|
In 2016, there were 437 opioid-related overdose deaths- a rate of 35.8 deaths per 100,000 persons nearly 3 times higher than the national rate of 13.3 deaths per 100,000. From 2013 through 2016, opioid-related deaths in New Hampshire tripled. NAS in New Hampshire increased dramatically from 2003 through 2011--from 20 cases in 2003 to nearly 150 in 2011. Between 2005 and 2015 the number of infants with NAS increased fivefold, rising from 52 to 269 infants (a rate of 24.4 of 1,000 live births) diagnosed with NAS. |
Dartmouth-Hitchcock MIR (regional): This is a model program providing support for pregnant and parenting women in recovery from opioid addiction. |
Clinical services provided for mothers:
Clinical services provided for children:
Other services:
|
| New Mexico | ||
|
In 2016, there were 349 opioid-related overdose deaths--in New Mexico--a rate of 17.5 deaths per 100,000 persons. The incidence of NAS in New Mexico has increased from 3.7 cases per 1,000 births in 2009 to 8.5 cases per 1,000 in 2013. As of 2016, ranks 29 for opioid related deaths of women. |
Centennial Home Visiting pilot program (statewide): includes the NFP and PAT. University of New Mexico Addiction and Substance Abuse Program (regional): central hub for treatment and intervention consultation for the provision of treatment of pregnant women with OUD. The program also works directly with Milagro, a program that offers prenatal care for women with OUD and has the ability to offer housing to women who require specialized services not available in their home area. Trainings and models of care offered through the centralized hub include information on women-specific services and best practice approaches. |
PAT services:
NFP services:
Milargo Program:
|
| North Carolina | ||
|
In 2016, there were 1,505 opioid-related overdose deaths--- in North Carolina--a rate of 15.4 deaths per 100,000 compared to the national rate of 13.3 deaths per 100,000 persons. Since 2010, when the rate was 8.1 deaths per 100,000 persons, the rate has almost doubled. |
CASAWORKS for Families Residential Services (statewide): 28 programs using evidence-based treatment models located in 13 counties across the state. CASAWORKS Programs for Women receiving Work First Cash Assistance (statewide): Programs for women who are mothers, require a residential level of substance abuse treatment, and receive Work First cash assistance. UNC Horizons (regional): offers residential and outpatient services the pregnant women with SUD. This includes meeting with a counselor or peer support specialist who will meet with the patient during and after the pregnancy, help the patient develop an individual treatment plan, provide information about substance use during pregnancy and after the baby is born, listen to the patient's concerns and work with her toward solutions, provide counseling for depression, anxiety, stress education and other issues, and refer interested patients to Horizons outpatient groups on treatment and recovery and parenting or to a residential program at Horizons or elsewhere in North Carolina. |
Programs for women who are: pregnant; or postpartum; or mothers and require a residential level of substance abuse treatment. Some programs are able to accommodate other children (up to age 11). Services typically include:
Services typically include:
UNC Horizons:
|
| Ohio | ||
|
Dramatic increase in NAS inpatient hospitalization rate per 10,000 live births in Ohio, 2004-2013. Increase from 20 per 10, 000 live births to over 120 per 10, 000 live births. State with 3rd highest rate of opioid deaths (32.9 per 100, 000 in 2016). State with one of the highest rate of opioid prescriptions per 100k in 2016 (85.8). |
Ohio NAS Infant Care Project (statewide): increase identification of and compassionate withdrawal treatment for full-term infant born with NAS and reduce lengths of stay across participating sites. MOMS Program (statewide): 2-year quality improvement initiative. MOMS program seeks to improve maternal and infant outcomes, promote family stability, and reduce costs of NAS. The strategy includes providing treatment to pregnant mothers with opiate issues during and after pregnancy through a MCH model of care. This team-based health care delivery model emphasizes care coordination and wraparound services. MCH model (statewide): patient-centered and team-based health care delivery model to engage and empower expecting mothers in coordinated care. MOMS Plus (MOMS+) (statewide): stemmed from MOMS and the goal for MOMS+ is to improve care and outcomes for the mother-infant relationship by supporting maternity care providers in the care of pregnant women with OUD, working closely with those who provide MAT and behavioral therapy. |
MOMS Services:
MCH model to include:
MOMS+ services include:
|
| Pennsylvania | ||
|
In 2016, there were 2,235 opioid-related overdose deaths in Pennsylvania; rate of 18.5 deaths per 100,000 persons. The state ranks fourth in opioid-related overdose deaths for women. While data are not available comparing Pennsylvania rates of NAS to nationwide rates, NAS events reported to the Pennsylvania Patient Safety Authority rose from 1 in 2005 to 221 in 2014 (Pennsylvania PSA, 2015), resulting in a total of 797 events during this time period. |
Magee's Pregnancy Recovery Center (regional): outpatient program offering PPW comprehensive and compassionate care for opioid addiction. Mothers Medication Assisted Treatment for Engagement and Resilience (Mothers MATTER) (regional): program offered at Penn Medicine's Perinatal COE that offers outpatient office-based buprenorphine treatment in an integrated setting with routine obstetric services and prenatal care to PPW with OUD. |
Magee's Pregnancy Recovery Center services include:
Mothers MATTER services include:
|
| Rhode Island | ||
|
Rhode Island is among the top 10 states with the highest rates of opioid-related overdose deaths. In 2016, there were 279 opioid-related overdose deaths in Rhode Island--a rate of 26.7 deaths per 100,000 persons and more than twice the national rate of 13.3 deaths per 100,000. The incidence of NAS in Rhode Island increased from 2.8 cases per 1,000 births in 2002 to 7.3 cases per 1,000 in 2012--a more than 2-fold increase. As of 2016, ranks 36 for opioid related deaths of women. |
Starbirth and Residential Treatment (regional): provide services to pregnant women and prioritize this population. Women's Day (regional): outpatient program that allows women to address addiction issues and work towards recovery while remaining at home to take care of their family. Project Link (regional): outpatient program that works with pregnant women and their children on health and recovery issues. |
Starbirth and Residential Treatment services:
Women's Day and Project link both offer these services:
|
| Texas | ||
|
In 2016, there were 1,375 opioid-related overdose deaths in Texas--a rate of 4.9 deaths per 100,000 persons compared to the national rate of 13.3 deaths per 100,000 persons. Since 2010, the number of heroin-related deaths steadily increased from 260 to 530 deaths, and deaths attributed to synthetic opioids (mainly fentanyl) rose from 156 to 250. |
The "Mommies" Program (statewide): a Model of Integrated Care is the coordinated of wraparound services to support PPW with any type of SUD and grew to also include MAT to PPW. Care is delivered in a collaborative, non-punitive, therapeutic manner that aims to support women who seek treatment and focuses on the best interests of the women. Collaboration also occurs between other service-providing agencies that may be working with the Mommies such as the Adult Probation Department and the Department of Family and Protective Services (Child Protective Services). |
In addition to MAT Offers behavioral health services including:
|
| Utah | ||
|
In 2016, there were 466 opioid-related overdose deaths in Utah --a rate of 16.4 deaths per 100,000 persons and more than the national rate of 13.3 deaths per 100,000 persons. The incidence of NAS in Utah has increased from 0.8 cases per 1,000 births in 2000 to 4.1 cases per 1,000 births in 2011, a more than 5-fold increase. As of 2016, ranks 28 for opioid related deaths of women. |
The Odyssey House, Inc. (regional): increased access to residential SUD treatment to PPW and their children in a family and client centered, trauma-informed treatment setting with access to a full spectrum of behavioral health service. |
The Odyssey House services:
|
| Vermont | ||
|
In 2016, there were 101 opioid-related overdose deaths in Vermont--a rate of 18.4 deaths per 100,000 persons and more than the national rate of 13.3 deaths per 100,000 persons. According to a CDC study, the incidence of NAS in Vermont has increased from 0.7 cases per 1,000 births in 2001 to 33.3 cases per 1,000 in 2013, an almost 48-fold increase. As of 2016, ranks 44 for opioid related deaths of women. |
Children and Recovering Mothers collaborative (CHARM) (statewide): includes 11 organizations that collectively provide comprehensive care coordination for pregnant women with opioid addiction and consultation for child welfare, medical, and addiction professionals across Vermont. |
CHARM services:
Special Supplemental Nutrition Program for Women, Infants, and Children
|
| Virginia | ||
|
In 2016, there were 1,130 opioid-related overdose deaths in Virginia--a rate of 13.5 deaths per 100,000 persons and 773 babies in Virginia were born with NAS, a rate of 8.0 cases per 1,000 births. The average across 28 states included in a separate 2013 analysis was 6.0 cases per 1,000 births. In 2015, Virginia providers wrote 70 opioid prescriptions per 100 persons (approximately 5.6 million prescriptions), equivalent to the national average. |
Phoenix House (regional): residential treatment program that offers comprehensive and professional drug and alcohol addiction treatment services for pregnant women and mothers and their young children in residential settings. They offer a flexible length of stay and a phased treatment regimen of individual, group, and family counseling sessions that are woman-centered and sensitive to the special needs of women who have experienced past traumas. |
Phoenix House services include:
|
| West Virginia | ||
|
State with highest rate of opioid deaths (43.3 per 100, 000 in 2016) This rate is up a low 1.8 deaths per 100,000 in 1999. State with one of the highest rate of opioid prescriptions per 100k in 2016 (110.0). NAS incidence rates per 1,000 hospital births, increased from 0.5 in 1999 to 33.4 in 2013. |
Lily's Place (regional): provides integrated and comprehensive prevention, early intervention, SUD treatment, and recovery support services for PPW with SUDs. Drug Free Moms and Babies Program (statewide): aims to support healthy pregnancy outcomes by providing integrated and comprehensive prevention, early intervention, SUD treatment, and recovery support services for PPW with SUDs. |
Lily's Place offers:
Drug Free Moms and Babies Program offers:
|
| Wisconsin | ||
|
The rate of opioid overdose deaths almost doubled from 2006 to 2015. As of 2016, ranks 17 for opioid related deaths of women. Wisconsin has seen substantial increase in NAS: 1.9 out of every 1,000 births in 2007 to 7.9 out of every 1,000 births in 2013. |
Pregnancy2Recovery (regional): program that partners with SSM Health and Safe Communities of Madison-Dane County Birth to 3 Program (statewide initiative): stemmed from the state amendment to increase case management that include comprehensive assessments and periodic reassessment of individual. Birth to 3 Program is covered under BadgerCare Plus. |
Specific for the case management for the Birth to 3 Program:
For BadgerCare Plus:
|
NOTES
-
Licensed physicians who have had a waiver to treat 100 patients for at least one year can become eligible for the patient limit of 275 hold board certification in addiction medicine or addiction psychiatry by the American Board of Addiction Medicine or the American Board of Medical Specialties, or certification by the American Board of Addiction Medicine or the American Society of Addiction Medicine. Most physicians could prescribe buprenorphine to up to 100 patients.
-
National Alliance of Advocates for Buprenorphine Treatment, Why are doctors limited as to how many people they can help with buprenorphine? https://www.naabt.org/faq_answers.cfm?ID=46, Accessed November 1, 2018.
-
Psychiatric News, Why Aren't More Physicians Prescribing Buprenorphine? https://psychnews.psychiatryonline.org/doi/full/10.1176/appi.pn.2016.PP3a2, Published March 4, 2016.
-
See https://www.samhsa.gov/sites/default/files/family_treatment_paper508v.pdf.
-
See https://ncsacw.samhsa.gov/files/Collaborative_Approach_508.pdf.
-
See http://nasadad.org/wp-content/uploads/2010/12/Guidance-to-States-Treatment-Standards-for-Women1.pdf.
-
The Family First Prevention Services Act permits the use of Title IV-E funds to prevent separation of children from their families and promotes family unification. Funds can be used to cover room and board costs for children residing in residential SUD treatment programs with a parent start October 2018.
-
Bureau of Drug and Alcohol Services, New Hampshire Department of Health and Human Services, Key Components for Delivering Community-Based Medication Assisted Treatment, Services for Opioid Use Disorder in New Hampshire. https://www.dhhs.nh.gov/dcbcs/bdas/documents/matguidancedoc.pdf.
-
See https://odh.ohio.gov/~/media/ODH/ASSETS/Files/cfhs/octpim/imsummit2016/….
-
See http://bh.medicaid.ohio.gov/Portals/0/Providers/20180530percent20BHperc….
-
See http://momsohio.org/child-welfare-worker/child-welfare-attributes/MOMSp….
-
In OUD treatment programs, child life specialists are degreed staff who educate PPW on how to identify and respond to infant cues.
FAMILY-CENTERED MEDICATION-ASSISTED TREATMENT
This report was prepared under contract #HHSP233201600021I between the U.S. Department of Health and Human Services (HHS), Office of Disability, Aging and Long-Term Care Policy (DALTCP) and the Research Triangle Institute. For additional information about this subject, you can visit the DALTCP home page at http://aspe.hhs.gov/office-disability-aging-and-long-term-care-policy-daltcp or contact the ASPE Project Officer, Kristina West, at HHS/ASPE/DALTCP, Room 424E, H.H. Humphrey Building, 200 Independence Avenue, S.W., Washington, D.C. 20201. Her e-mail addresses is: Kristina.West@hhs.gov.
Reports Available
Expanding Access to Family-Centered Medication-Assisted Treatment Issue Brief
- HTML: https://aspe.hhs.gov/basic-report/expanding-access-family-centered-medication-assisted-treatment-issue-brief
- PDF: https://aspe.hhs.gov/pdf-report/expanding-access-family-centered-medication-assisted-treatment-issue-brief
State Policy Levers for Expanding Family-Centered Medication Assisted Treatment
