Analysis of State Efforts to Comply with Fair Labor Standards Act Protections to Home Care Workers
Pamela J. Doty, Ph.D., and Marie R. Squillace, Ph.D.
Office of the Assistant Secretary for Planning and Evaluation
U.S. Department of Health and Human Services
Edward Kako, Ph.D.
Mission Analytics Group, Inc.
December 2019
Printer Friendly Version in PDF Format (36 PDF pages)
ABSTRACT
The purpose of this study is to describe and document changes states have made to their Medicaid or other publicly-funded consumer directed home care programs for seniors and individuals with disabilities to comply with the 2013 update to Fair Labor Standards Act (FLSA) regulations. This report provides an overview of early implementation activities at the state level and perspectives from various stakeholder groups. After introducing the study methods, we describe issues that emerged from interviews conducted with stakeholder group representatives. We then present findings from an environmental scan of state policies and procedures conducted in all U.S. states, including the District of Columbia. Finally, to illustrate both state variations in FLSA implementation and promising practices, we present examples of select case study states with well-documented hardship exceptions policies: California, Massachusetts, Wisconsin, and Ohio; and provide insights from all case studies. This report, prepared by ASPE staff, synthesizes and expands upon key study findings from several reports prepared by Mission Analytics.
This report was prepared under contract #HHSP233201600018I between HHS's ASPE/DALTCP and Mission Analytics Group, Inc. For additional information about this subject, you can visit the DALTCP home page at http://aspe.hhs.gov/office-disability-aging-and-long-term-care-policy-daltcp or contact the ASPE Project Officer, Marie Squillace, at HHS/ASPE/DALTCP, Room 424E, H.H. Humphrey Building, 200 Independence Avenue, S.W., Washington, D.C. 20201. Her e-mail address is: Marie.Squillace@hhs.gov.
DISCLAIMER: The opinions and views expressed in this report are those of the authors. They do not reflect the views of the Department of Health and Human Services, the contractor or any other funding organization. This report was completed and submitted on September 5, 2019.
TABLE OF CONTENTS
- Home Care Rule Requirements
- Medicaid Self-Directed Aide Services
- Why Focus Exclusively on Implementation of Department of Labor Home Care Rule for Self-Direction
- Financial Management Services
- Potential Medicaid Cost Consequences of Fair Labor Standards Act Implementation
- Research Questions
- Key Informant Interviews
- Environmental Scan
- Case Studies
- Limits on Workers' Hours
- Exceptions Policies
- Budget Authority
- Live-In Domestic Service Employee Exemption
- Insights from Case Studies
LIST OF FIGURES
LIST OF TABLES
- TABLE 1: Wisconsin Home Care Overtime Exception Policies
ACRONYMS
The following acronyms are mentioned in this report.
| ASPE | HHS Office of the Assistant Secretary for Planning and Evaluation |
|---|---|
| AwC | Agency with Choice |
| CDPAP | Consumer Directed Personal Assistance Program |
| CDSS | California Department of Social Services |
| CMS | HHS Centers for Medicare & Medicaid Services |
| CoC | Continuity of Care |
| D/B/A | Doing Business As |
| DOJ | U.S. Department of Justice |
| DOL | U.S. Department of Labor |
| F/EA | Fiscal/Employer Agent |
| FFS | Fee-For-Service |
| FLSA | Fair Labor Standards Act |
| FMS | Financial Management Services |
| HCBS | Home and Community-Based Services |
| HHS | U.S. Department of Health and Human Services |
| ICS | Independence Care Systems |
| IHSS | In-Home Supportive Services |
| IRIS | Include, Respect, I Self-Direct policy manual |
| LTSS | Long-Term Services and Supports |
| MACPAC | Medicaid and CHIP Payment and Access Commission |
| MCO | Managed Care Organization |
| MLTSS | Managed Long-Term Services and Supports |
| NASDDDS | National Association of State Directors of Developmental Disabilities Services |
| NASUAD | National Association of States United for Aging and Disability |
| NYLL | New York Labor Law |
| PASSPORT | Pre-Admission Screening System Providing Options and Resources Today waiver |
| PCA | Personal Care Attendant |
| SSA | Service and Support Administrator |
| WPCS | Waiver Personal Care Services |
INTRODUCTION
The purpose of this study is to describe and document changes states have made to their Medicaid or other publicly-funded consumer directed home care programs for seniors and individuals with disabilities to comply with the 2013 update to Fair Labor Standards Act (FLSA) regulations. This report provides an overview of early implementation activities at the state level and perspectives from various stakeholder groups. After introducing the study methods, we describe issues that emerged from interviews conducted with stakeholder group representatives. We then present findings from an environmental scan of state policies and procedures conducted in all states, including the District of Columbia. Finally, to illustrate both state variations in FLSA implementation and promising practices, we present examples of select case study states with well-documented hardship exceptions policies: California, Massachusetts, Wisconsin, and Ohio; and provide insights from all case studies. To carry out this study, the U.S. Department of Health and Human Services (HHS) Office of the Assistant Secretary for Planning and Evaluation (ASPE) contracted with Mission Analytics. This report, prepared by ASPE staff, synthesizes and expands upon key study findings from several reports prepared by Mission Analytics.
BACKGROUND
Home Care Rule Requirements
On October 1, 2013, the U.S. Department of Labor (DOL) issued a final rule (the Home Care Rule) to update regulations concerning the FLSA domestic service employee exemptions. The Home Care Rule extended minimum wage and overtime protections to most home care workers, to ensure that they had the same basic wage protections as most United States workers, including those who provide similar types of assistance to people with disabilities residing in nursing homes and group homes.
In 1974, Congress extended the minimum wage and overtime pay protections of the FLSA to "domestic service" employees such as cooks, housekeepers, maids, or gardeners employed in households. However, this same legislation included a "companionship exemption" for domestic service employees providing companionship services, which was defined broadly by regulation and therefore understood to include personal care to seniors and people with illnesses, injuries, or disabilities. It also exempted from overtime pay requirements all categories of domestic service workers who live in the household in which they provide services (the "live-in domestic service employee exemption").
The 2013 Home Care Rule revised the definition of companionship services to clarify and narrow the duties that fall within that category. To qualify for the companionship exemption from minimum wage and overtime pay requirements, home care workers may only provide limited amounts of assistance with personal care tasks (such as bathing, dressing, toileting, transferring into and out of beds and chairs) and household help (cooking, cleaning, laundry), and no medical help that would normally be provided by a licensed nurse or therapist. The Rule also provided that third party employers, such as home care agencies or any other joint employers who share employer responsibilities with individual household employers, cannot claim either the companionship services exemption or the live-in domestic service worker exemption. Depending on the design of publicly-funded home care programs, courts could deem government agencies and/or their administrative contractors to be joint employers under the FLSA, along with self-directing public program participants who hire and supervise individual home care workers instead of relying on home care agencies for aide services.
Although issued in 2013, the Home Care Rule had an effective date of January 1, 2015. The intent was to give states time to prepare to implement the Rule. DOL led an extensive implementation effort to help employers of home care workers prepare for FLSA compliance. Due to litigation, DOL did not begin enforcement of the Home Care Rule until November 12, 2015. Because of the many months of legal uncertainty as to whether the Rule would be upheld by the courts, states in many cases delayed planning for implementation. As a result, postponement of the Rule's effective date and DOL enforcement did not result, as intended, in states taking the additional time to decide how to implement the Home Care Rule.
After DOL's promulgation of the Home Care Rule, the U.S. Department of Justice (DOJ) together with HHS's Office of Civil Rights and, separately, the HHS Centers for Medicare & Medicaid Services (CMS) issued written guidance to states.[1] The guidance urged states to take care in implementing the Home Care Rule to ensure that efforts to contain potential Medicaid cost increases did not have the unintended consequence of exacerbating rather than alleviating worker shortages and adversely affecting Medicaid program participants' access to home care aide services.[2] The guidance specifically counseled states to avoid imposing a 40-hour hard cap limiting the Medicaid billable hours per week that workers employed by self-directing program participants would be permitted to work, with no or only very restricted exceptions. The guidance cautioned states that if they limited workers' hours to 40 per week without hardship exceptions this could result in putting Medicaid program participants living at home at high risk of requiring nursing home placement or other adverse consequences associated with unmet needs for assistance with daily living tasks. By doing so, states might subsequently be determined to have violated the Supreme Court's 1999 Olmstead ruling affirming the rights of people with disabilities of all ages under the 1990 Americans with Disabilities Act to receive Medicaid or other disability-related publicly-funded services to which they were otherwise entitled in non-institutional settings unless medically contra-indicated.[3] The CMS guidance reminded states of the assurances they were required to make under Medicaid law and regulations with regard to safeguarding the health and well-being of Medicaid home and community-based services (HCBS) recipients.
Medicaid Self-Directed Aide Services
Self-direction of home care aide services is an alternative to relying on home care agencies to assign and supervise aides whose terms of employment the agency generally controls. Agencies recruit and train the aides they employ and these aides have rarely had any previous acquaintance with the clients. In contrast, self-directing program participants recruit, schedule, and supervise individual workers of their choosing, who are often family members and friends. Self-directing program participants typically take either full or at least partial responsibility for training or arranging customized training for their workers. Self-directing program participants have the right to dismiss their aides at will. Recruiting aides may be difficult for both traditional home care agencies and self-directing program participants. Medicaid beneficiaries with disabilities who choose to self-direct often benefit from having more choice and control over their aide services. They may still find the aide recruitment process difficult and time-consuming.
Although Medicaid is the source of payment, self-directing program participants, unlike agency clients, must always approve their workers' timesheets before workers are paid. In some self-direction programs, self-directing program participants have no control over their workers' hourly wage rates. These wage rates are fixed via a state provider rate setting process, which in some states involves collective bargaining with a union representing participant-directed workers. Program participants may purchase up to the maximum number of aide hours authorized for them by their Medicaid case managers, but if they do not access all of those hours they lose and cannot "bank" their unused hours for later use.
However, in self-direction programs that allow program participants to exercise "budget authority," program participants have leeway to decide, within the monetary limits of their budgets, how many hours of aide services to purchase at what hourly wage rates. Typically, they are permitted to carry unspent funds over from month to month, which enables them, for example, to vary their use of paid services somewhat. For example, they may prefer to arrange to have extra paid aide hours available when family caregivers who provide significant amounts of unpaid help need to take a break.
Why Focus Exclusively on Implementation of Department of Labor Home Care Rule for Self-Direction?
Nearly one million people -- approximately one-in-four Medicaid recipients of personal care aide services -- are estimated to be participating in self-directing programs in Medicaid or other state-funded programs. As of 2016, every state (including the District of Columbia) had at least one Medicaid-funded self-directed services program.[4] Additionally, self-direction, although not the most common personal assistance services delivery mode, attracts Medicaid program participants with higher than average disability-related needs. Such individuals are at higher than average risk of requiring institutional care if they cannot get their needs adequately met at home. Medicaid is most likely to authorize aide coverage in excess of 40 hours per week for such "high need" individuals.
Financial Management Services
Medicaid almost never authorizes reimbursement to program participants rather than service providers, so self-directing program participants cannot pay their workers directly. Medicaid provides for financial management services (FMS) entities (sometimes also referred to as fiscal intermediaries) to pay self-directing program participants' workers. States may arrange for FMS through a "fiscal/employer agent" (F/EA) in which the FMS is strictly a payroll agent and self-directing program participants are their workers' sole legal employers under tax law. Alternatively, states may arrange for FMS via an "Agency with Choice" (AwC). Although, for tax purposes, the AwC is the sole legal employer of self-directing program participants' workers; AwCs do not assume all of the other employer responsibilities of a typical home care agency. In both models, self-directing program participants continue to recruit, schedule, and supervise their individual workers. States may elect either the F/EA or the AwC approach to FMS, but some offer both models and allow self-directing program participants to choose between them.
Unlike tax law, the FLSA allows for the possibility that a worker may have multiple employers, each jointly and severally liable for wages owed. For purposes of FLSA compliance, an AwC model of FMS may often be a third party employer, whereas an F/EA that acts strictly as a payroll agent is often not a third party or a joint employer with the program participant for FLSA purposes. In either case, other entities (such as state and/or local government agencies) may be deemed joint employers. Such determinations are always made on a case-by-case basis.
Potential Medicaid Cost Consequences of Fair Labor Standards Act Implementation
After the Home Care Rule went into effect, most self-directing program participants' employees became entitled to overtime pay. As a result, they could enjoy higher earnings if Medicaid program rules authorized them to work for more than 40 hours per week.
Because pay increases for workers attributable to the Home Care Rule result in higher Medicaid expenditures for personal care services, states have a financial incentive to take steps to limit the possibility of Medicaid cost increases associated with overtime and travel time pay liability. They may do so primarily by limiting the number of Medicaid reimbursable service hours that self-directing program participants' aides are permitted to provide per week. Doing so does not reduce the amount of covered aide hours authorized for individual program participants based on their needs assessment, but could require them to recruit additional workers in order to obtain all of their authorized coverage. For example, states might adopt highly restrictive policies (such as a "hard cap" limiting worker hours to a maximum of 40 Medicaid reimbursable hours per week).
Where a common third party joint employer exists, the hours worked for multiple program participants/employers must be aggregated and overtime pay is required if the total exceeds 40 hours per week. Potential cost increases related to overtime pay and travel time pay are greater when home care workers are determined to have third party employers and when program rules permit home care workers to work more than 40 hours per week. Accordingly, states seeking to curb costs associated with overtime and travel time pay have a financial incentive to cap workers' Medicaid reimbursable hours and/or structure their self-direction programs such that self-directing program participants are their workers' sole employers. They might, for this reason, take care not to allow organizations or government agencies to take on employer functions likely to result in their designation as third party employers.
Two self-direction program design and implementation choices, in particular, can significantly affect FLSA-related Medicaid costs:
-
Use of FMS entities that facilitate payment of Medicaid monies to compensate self-directing program participants' workers.
-
Whether to grant self-directing program participants "budget authority" that allows them to negotiate with their aides how many hours per week they will work and their hourly wages.
Research Questions
This exploratory study addressed the following key research questions:
-
Among key informants with a national perspective on the issues that might arise with home care, what were the concerns and expectations about the impact of the Home Care Rule?
-
Based on publicly available documents, how did states implement the Home Care Rule? For example:
-
To what extent did states cap Medicaid billable worker hours at 40 hours per week or, alternatively, at some higher number of hours that would allow for some overtime pay without program participants having to request special permission?
-
Did states develop exceptions policies to allow self-directing program participants to obtain permission, based on their special needs, to employ individual workers in excess of the weekly cap on the number of hours?
-
Did states allow self-directing program participants to exercise budget authority self-direction that would give them more flexibility about how many aide hours to purchase and hourly wage rates?
-
Did states permit self-directing participants to claim the live-in exemption for family members or other paid caregivers who live with them?
-
-
Based on case studies of selected states, what did we learn about promising practices and the ways in which the Home Care Rule interacted with local conditions?
METHODS
Key Informant Interviews
The first phase of the study consisted of interviews with stakeholder group representatives at the national level. These included: Advocates for home care workers (National Employment Law Project and PHI); Advocates for people with disabilities and self-directing Medicaid program participants (ADAPT, National Council on Independent Living, the Arc, ANCHOR, and Center for Public Representation); staff of associations representing state program administrators (Medicaid Directors Association, National Association of States United for Aging and Disability [NASUAD], and National Association of State Directors of Developmental Disabilities Services [NASDDDS]); and experts who specialize in providing technical assistance to states on the design of their self-direction programs and on FLSA implementation (Applied Self Direction). NASUAD, NASDDDS, and Applied Self Direction were also subcontractors on the research study and assisted with data collection for the environmental scan.
We specifically asked key informants about their organization and their role in it; their view of the landscape for home care prior to the DOL rule; expectations for the impact of the Home Care Rule on consumers and workers; their organization's role in responding to the Notice of Proposed Rulemaking; and expectations for their organization's work related to the rule going forward.
We developed a common protocol for all key informant telephone discussions, which we tailored where possible to the organization's mission and history. The protocol was followed as closely as possible while allowing enough flexibility to follow interesting and important or unexpected lines of inquiry.
Environmental Scan
The environmental scan served as our primary data source for collecting information on FLSA implementation in all states, including the District of Columbia. Data were collected on self-directed home care programs from the period January 2017 - July 2019. Documentation came from several sources, including but not limited to: state informational web pages; state administrative codes; state-issued letters to self-directing participants or their home care workers; and manuals prepared for participants or for workers that set out the requirements for receiving services from, or working in, the self-directed home care program. There are more than 200 programs across the country that offer self-direction and vary in size. We found information on approximately 75 programs and almost always included the largest program in the state. Project subcontractors -- who were particularly knowledgeable about some states -- provided additional information through their direct state contacts to assist in filling in the blanks, where needed.
Case Studies
Case studies were conducted in California, Massachusetts, Minnesota, New York, Ohio, and Wisconsin. Sites were selected from among those recommended by key informants to illustrate both state variations in FLSA implementation and adoption of promising practices. The latter represent efforts to balance the various interests of states, self-directing Medicaid beneficiaries, and their individual workers.
To inform the case studies, we reviewed policies and procedures documents; read accounts of decisions about how implementation were made and about the changing landscape of community long-term services and supports (LTSS) in the states more broadly; reviewed the websites of advocacy organizations; collected reports issued by non-profit organizations; and queried informants with insight on the implementation process in their states.
STAKEHOLDER OBSERVATIONS
Key informants made a number of observations about the Home Care Rule. Some of these were predictions, expectations, hopes, and/or concerns:
Several stakeholders predicted that all or most states would set limits on how many hours home care workers in self-directed services programs would be allowed to work per week in order to restrict Medicaid cost increases resulting from the FLSA's overtime pay requirement. Consumer advocates were more inclined toward pessimism than other key informants were; that is, to predict that many states would set a "hard cap" of 40 hours with no or few hardship exceptions to avoid or minimize Medicaid expenditure increases attributable to the Home Care Rule's overtime pay requirement. Consumer advocates also feared that states might find it expedient to eliminate self-direction as an option altogether.
State association representatives noted that some of their members had supported the Rule whereas others had opposed it as likely to result in Medicaid expenditure increases state officials claimed their states could not afford. They (the Medicaid Directors Association, in particular) predicted that the "line of least resistance" would be for states to limit Medicaid expenditure increases that might result from overtime pay liability by limiting individual workers' Medicaid billable hours. Prior to issuance of the Home Care Rule, associations representing state agencies had urged DOL to postpone the effective date and the beginning of DOL's enforcement of the Rule beyond the usual timeframe for final regulations. The associations' reasoning was that this would give governors and state legislatures more time to prepare to comply. They believed more lead time might increase the likelihood that states would appropriate additional funding to allow for increased Medicaid expenditures associated with paying overtime and, if required, travel time and to retool administrative processes to ensure compliance. However, the state agency associations were aware that states had postponed planning while opposition to the Home Care Rule was being litigated and did not resume planning until it was clear that the Rule would not be overturned.
Advocates for people with disabilities were more likely to voice concerns that the Home Care Rule could -- and likely would -- have unintended negative consequences for both self-directing program participants and their individual workers. They expected negative consequences to result if states chose to cap worker hours and, especially, if they set the limit at 40 hours per week with no or few hardship exceptions. Doing so could exacerbate worker shortages, putting Medicaid beneficiaries at greater risk of adverse consequences such as not being able to find workers to provide the full amount of their authorized aide hours. As a result, individuals with severe disabilities could experience unmet needs for assistance that would jeopardize their health and safety in the community and put them at increased risk of institutionalization. They also believed states' decisions to limit workers billable hours could also have unintended adverse effects on workers. This would result, for example, if workers who had previously worked hours for which they were now entitled to overtime pay could no longer work hours that incurred overtime pay liability. Not only would these workers not benefit from receiving overtime pay, their weekly earnings would decrease.
Some stakeholders and disability advocates predicted that states would make design changes to their self-directed services programs to grant self-directing program participants budget authority that would allow hem to decide how many hours of aide service to purchase in total and from individual workers and at what hourly rate (which might differ for different workers). Their reasoning was that this would lessen the potential for Medicaid cost increases by reducing the likelihood of joint employment determinations. They noted that a few states had already done so, and in these states, the shift to budget authority self-direction allowed self-directing program participants to maintain continuity of care (CoC) by avoiding having to cut the hours of a live-in worker (typically co-residing paid family caregivers) who had previously been regularly working more than 40 hours per week.[5]
Several stakeholders expected states to change their approach to providing FMS that enable Medicaid beneficiaries to self-direct their aide services in response to the Home Care Rule. Some expected states to move away from the AwC model toward the F/EA approach. Their reason for doing so would be to curb the potential for Medicaid cost increases associated with third party employers. Other stakeholders predicted the opposite -- a shift away from F/EA in favor of AwC -- although their reasons for expecting states to make such a change were less clear.[6]
FINDINGS
Limits on Workers' Hours
Based on data collected during the environmental scan, states were grouped into two main categories according to limits set on workers' hours: states that capped weekly hours at 40, and those that allowed workers to work more than 40 hours per week. Some states were difficult to classify. For example, if states prohibited program participants exercising budget authority from having workers work more than 40 hours per week or required them to obtain prior authorization to do so, we classified those states in the 40 hours category, even if they had robust exceptions policies (e.g., Wisconsin). We included states in the latter category if the state had an explicit policy that allowed for a specific number of overtime hours without special permission. Examples include California, Massachusetts, and Ohio. We also included in the 40+ category states that allowed self-directing program participants exercising budget authority to allow workers to work more than 40 hours per week if they could pay overtime without over-spending their budgets.
| FIGURE 1. States with Work Week Hour Caps |
|---|
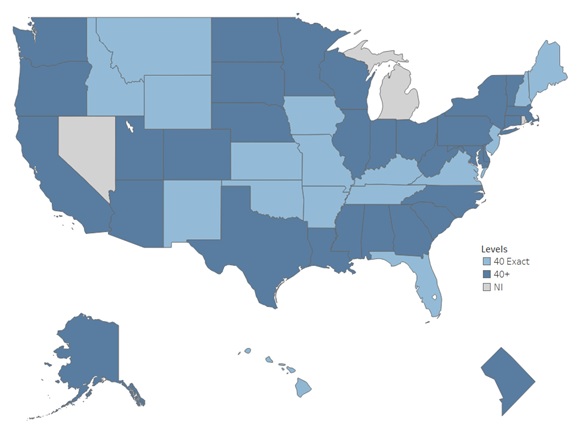 |
Additionally, we classified in the 40+ hours category states that delegated the authority to allow or disallow requests for individual workers to work hours requiring overtime pay to managed care entities or to FMS entities. Finally, we designated in the 40+ hours category states with employer authority only self-direction programs that allowed program participants to have live-in workers when the evidence (e.g., payment of travel time) indicated that the state was a joint employer not eligible to take the live-in exemption to the overtime pay requirement (e.g., Oregon).
Figure 1 shows the limits on workers' hours by state according to our classification scheme. Thirty-two states (including the District of Columbia) allowed workers to work more than 40 hours per week. Sixteen states limited the weekly number of hours to 40. We were unable to classify three states due to insufficient information.
Among the states that set the weekly hours cap at something greater than 40, there was considerable variation in the number of hours per week that aides could work without special permission. California was the most generous, with the limit on overtime pay for workers being the same as the authorized coverage limit for individual beneficiaries. In most other states with explicit limits on routine overtime, the typical cap was 45-50 hrs.
Exceptions Policies
Seventeen states have an exceptions policy for individuals who need more hours of home care service than the state's cap on worker hours ordinarily allows; however, the information on exceptions policy is limited (e.g., we could not determine the exception policy in 24 states) (Figure 2).
| FIGURE 2. States with Exception Policies |
|---|
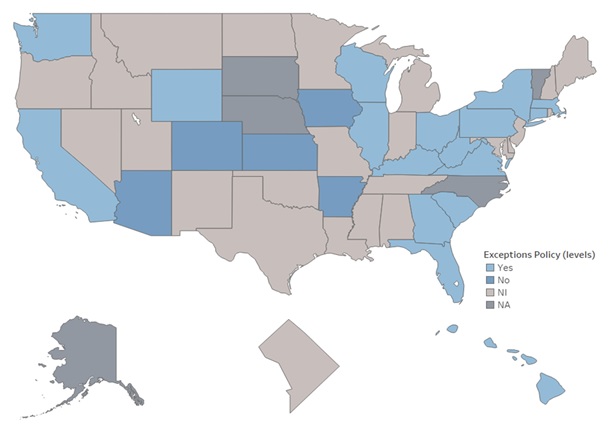 |
Apart from California, Massachusetts, Wisconsin, and Ohio, this study found few examples of states with well-documented hardship exceptions policies. More common are less well-defined exceptions to caps on worker hours such as those found in Kentucky (temporarily for emergencies), Wyoming (only if no other worker available), and in Hawaii (if approved by the individual's case manager and included in the Individual Support Plan). Also, in New York exceptions are determined on a case-by-case basis by managed care plans, and, therefore, there were no state mandated exceptions policies in this case. Below are descriptions of select case study states with well-documented exception policies:
California
California has a long-standing coverage limit of 283 hours per month on the number of provider hours an In-Home Supportive Services (IHSS) program participant can receive. The number of hours authorized for each program participant is determined by an individualized needs assessment which a social worker conducts using a standardized state assessment instrument and hours allocation formula. The cap on worker hours imposed after the Home Care Rule went into effect mirrors the IHSS coverage limit for individual program participants. Based on a 30-day month, the maximum number of hours a provider may work per week is 66 -- the standard 40 plus 26 hours of overtime. Home care workers employed by just one consumer can work up to the consumer's maximum hours divided by 4, or 70.75 hours. This difference is intended to provide added hours to paid family caregivers who live in the same household, who are nearly always on call, whether they are being paid or not.
To ensure CoC and to allow IHSS recipients to remain safely in their homes, California Department of Developmental Services established exceptions for limited, specific circumstances that allow the maximum weekly hours to be exceeded. These exceptions apply to IHSS-funded and also to supplemental aide hours above the IHSS coverage cap that might be authorized for IHSS recipients under HCBS waiver or state plan programs. Because California is designated a joint employer, aide hours that a worker provides to one or more Medicaid beneficiaries must be an aggregated count toward overtime pay liability, regardless of the Medicaid state plan or waiver funding authority.
Exception 1: Live-In Family Care Providers Exception
IHSS providers may provide services to two or more live-in family member recipients and work up to 90 hours per work week, not to exceed 360 hours per month, provided they met the following requirements on or before January 31, 2016:
-
The provider works for two or more recipients.
-
The provider lives in the same home as all the recipients for whom he or she provides services.
-
The provider is related to all the recipients for whom he or she provides services, as a parent, adoptive parent, step-parent, grandparent or legal guardian. Recipients whose providers qualify for this exemption and work the maximum monthly 360 hours must hire other IHSS workers as necessary to provide supply the balance of hours.
According to a July 2018 California Department of Social Services (CDSS) Report to the Legislature, an average of 1,357 providers were approved for Exception 1.[7]
Exception 2: Extraordinary Circumstances Exception
Allows providers who serve two or more recipients to work up to 360 hours per month, up to 90 hours per week combined for all recipients, and not receive a work week violation, provided they meet at least one of the following three criteria:
-
Criteria A: Have complex medical or behavioral needs that must be met by a provider who lives in the same home as the recipient.
-
Criteria B: Live in a rural or remote area where available providers are limited, making it difficult for the recipient to hire another provider.
-
Criteria C: Be unable to hire a provider who speaks the same language to direct his or her care.
Under Criteria A, the IHSS provider must live in the same home as the recipient(s) applying for Exception 2 under this condition. Under Criteria B and C, the IHSS provider is not required to live in the same home as the recipient(s) applying for Exception 2 under these conditions. According to a July 2018 CDSS Report to the California Legislature, an average of 86 providers received Exception 2.[7]
Exception 3: Waiver Personal Care Services (WPCS) Exception
Some high need Medicaid beneficiaries need more than the 283 hours per month that is the maximum number of authorized hours per program participant (coverage limit) for IHSS. Such individuals may also be enrolled in HCBS waiver programs that will allow them to receive additional personal care aide hours above the IHSS coverage cap. Providers who work for such individuals may work up to 360 hours per month in combined hours authorized under Medicaid waivers and IHSS. On average, per month over the 24-month period FY 2016 - 2018, 735 IHSS/WPCS providers were approved for this overtime exemption.[7]
In total, nearly one-in-four IHSS workers regularly work more than 40 hours per week and receive overtime pay, most of them because of the generous regular limits rather than because of hardship exceptions to those limits.
Massachusetts
Participant-directed aides in Massachusetts may work up to 50 hours per week (10 hours of which incur overtime pay liability) without special approval. These limits apply both to aides employed by self-directing program participants in the fee-for-service (FFS) system and those employed by self-directing program participants who have voluntarily enrolled in Massachusetts' two Medicaid managed care programs: Senior Care Options or One Care.
Temporary Approvals
A consumer may request a temporary approval to schedule a personal care attendant (PCA) for more than 50 hours because:
-
The consumer has planned travel, and it would not be feasible to bring multiple PCAs along to provide services.
-
The consumer's PCA is temporarily unavailable (e.g., due to vacation or family leave).
-
The consumer has a temporary need (e.g., post-acute hospitalization).
-
The consumer's PCA works more than 66 hours per week and the consumer needs time to hire additional PCAs (to ensure that services can be provided safely and to ensure that no one PCA is working more hours per week than the state will allow).
Continuity of Care (CoC) Approvals
A consumer may request a CoC approval to schedule a PCA to work overtime when the consumer:
-
Has complex medical needs that require the services of the experienced PCA.
-
Has communication barriers that require the specialized skills of the experienced PCA.
-
Has specialized medical conditions that require fewer PCAs -- for example, when the consumer has a compromised immune system, and it is important to minimize the number of PCA with whom he or she comes into contact.
CoC approvals last for the duration of the consumer's prior authorization and must be resubmitted for each subsequent prior authorization period. For health and safety reasons, CoC approvals are limited to 66 hours per worker. A special form of CoC approval is granted in a "One-on-One Relationship" if the consumer:
-
Is approved for between 50 and 66 hours of PCA services per week.
-
Has one PCA who provides all the consumer's PCA services.
-
Resides together with the PCA (as confirmed via third party documentation).
Wisconsin
Wisconsin's exception policies are summarized in Table 1 in "bands" of overtime (40.25 hours to 60 hours, versus more than 60 hours); ongoing versus short-term; and type of self-direction (self-directed personal care, or SPDC, versus others). Wisconsin's policies are articulated in considerable detail in two manuals: the Include, Respect, I Self-Direct (IRIS) Policy Manual, and the IRIS Policy Manual: Work Instructions.[8]
| TABLE 1. Wisconsin Home Care Overtime Exception Policies | |||
|---|---|---|---|
| Exception Request Type | Hours Caregiver Working per Work Week | Live-In Caregiver | Non-Live-In Caregiver |
| Ongoing | 40.25-60.0 hours | Allowed | Allowed |
| Ongoing | Over 60 hours | Allowed | (Not Allowed) |
| Short-Term ( 60 days) | 40.25-60.0 hours | Allowed | Allowed |
| Short-Term ( 60 days) | Over 60 hours | Allowed | Allowed |
| SPDC Services Only Ongoing | 40.25-60.0 hours | Allowed | (Not Allowed) |
| SPDC Services Only Ongoing | Over 60 hours | Allowed | (Not Allowed) |
| SPDC and Other Services Ongoing | 40.25-60.0 hours | Allowed | Allowed |
| SPDC and Other Services Ongoing | Over 60 hours | Allowed | (Not Allowed) |
| SPDC/Other Services Short-Term ( 60 days) | 40.25-60.0 hours | Allowed | Allowed |
| SPDC/Other Services Short-Term ( 60 days) | Over 60 hours | Allowed | Allowed |
Key Points in Table 1:
-
The current cap is set at 60 hours per week. Live-in caregivers either may exceed that limit on a short-term basis or continuously, provided certain conditions are met.
-
Caregivers who do not live with the consumer can exceed 60 hours per week only for short periods. They can never exceed that cap on an ongoing basis.
Ohio
Ohio's exception policies are codified in state regulations (5123:2-9-03).[9] Once Independent providers have worked 60 hours in a work week providing Medicaid-funded services, they can only work more hours in two situations:
-
If the additional hours have been authorized by the consumer's service and support administrator (SSA) through the county board of developmental disabilities.
-
If there is an emergency.
Consumers and their care teams must try to identify any "known or anticipated events or circumstances" that would cause an independent provider to work more than 60 hours in a work week. These "events and circumstances" and any authorizations to work more than 60 hours should be documented in a person's individual service plan. Some "events and circumstances" include cases where:
-
The individual or his or her family member or provider has surgery or travel scheduled.
-
The individual has holidays or scheduled breaks from school.
-
The individual has a compromised immune system and may be put at risk by having additional providers.
-
The independent provider is the only provider trained by a nurse to perform delegated tasks or trained by a behavioral specialist to implement unique behavioral support strategies.
-
There is a shortage of other available providers.
In the latter two cases, the SSA must work with consumers and their care teams to develop a plan to change these circumstances. That could mean training another provider, finding an additional provider, or relying more on family members and other supports. If, after working in good faith, consumers cannot meet their home care needs, the SSA may give authorization for the independent provider to work more than 60 hours in a work week. The Ohio Home Care Rule defines an emergency as the "unanticipated and sudden absence of an individual's provider or natural supports due to illness, incapacity or other cause." If an independent provider has worked more than 60 hours because of an emergency, he or she must notify the individual's SSA within 72 hours of the event that created the emergency and report the number of hours they worked more than the 60-hour limit.
Under the Rule, independent providers must tell an individual's SSA how many people they provide Medicaid-funded services for, and the number of hours they work for such persons in total. Independent providers must provide this information when:
-
They are hired.
-
An emergency causes them to work more than 60 hours in a week.
-
The SSA asks for it.
Independent providers who violate the requirements of the Rule may have their certification denied, suspended, or revoked.
Budget Authority
Thirteen states (Alabama, Arizona, Colorado, Florida, Georgia, Kansas, Illinois, Louisiana, Minnesota, New Jersey, North Carolina, Texas, and West Virginia) allow self-directing program participants exercising budget authority to authorize overtime pay if they have sufficient funds in their budgets to cover the costs. Two of these states (Florida, New Jersey) require program participants to request special permission to use their funding for this purpose.
It is noteworthy, however, that where states allowed self-directing program participants with budgets to pay overtime rates if they could afford to do so, we did not find much evidence of states increasing the size of their budgets. In some cases (e.g., Alabama) paying overtime via a budget is technically allowable but appears to be rare because the amount of funding provided to self-directing program participants exercising budget authority is based on the assumption that they need less than 40 hours per week of aide services.
Self-directing program participants and their workers generally wish to avoid having workers who had previously been working hours for which overtime must now be paid to lose hours and therefore weekly earnings. There are a number of potential ways for those exercising budget authority to protect their workers from losing pay because of state efforts to limit Medicaid expenditure increases due to overtime pay. However, whether a particular method can be used depends on the circumstances, such as: whether the budget allocation provides funding that could be used to pay workers or to access other goods and services at the discretion of the budget holder, whether workers are live-in, and whether paid workers are family members who are permitted to also provide unpaid assistance, which non-family members may not.
Another possible motivation for states to redesign their programs to offer budget authority is they believe doing so might lessen the potential for Medicaid cost increases by reducing the likelihood of joint employment determinations. It is clear that some states did change their program designs to allow self-directing program participants to exercise budget authority following the issuance of the Home Care Rule. However, we were unable to determine whether their motivation for doing so was to avoid a joint employer designation.
Live-In Domestic Service Employee Exemption
Eleven states (Colorado, District of Columbia, Georgia, Illinois, Kansas, New Jersey, Pennsylvania, Vermont, Virginia, West Virginia and Wisconsin) allow claiming of the live-in exemption to the overtime pay requirement and 26 states do not (with unknown information on the remaining states). In states where taking the live-in exemption is not allowed but workers may be permitted to work for more than 40 hours per week, live-in paid home care workers of Medicaid beneficiaries working more than 40 hours in a work week will be paid overtime up to the limit on weekly hours, the same as non-live-in workers. This pattern may have emerged if states have carried out an analysis determining that these workers likely have one or more third party employers (perhaps the state itself) that are not entitled to claim the exemption. Alternatively, states may be unsure about whether they or some other entity might later be legally determined to be joint employers. Failure to pay overtime to live-in workers in such cases could entail paying substantial sums in back overtime pay, plus penalties. Anecdotal reports suggest that, indeed, some states have chosen not to allow the live-in exemption for this reason. However, live-in workers are usually family members and some states have adopted a policy that prohibits family members (whether live-in or not) from being paid for more than 40 hours per week.
Insights from Case Studies
Advocacy Played a Major Role in Implementation Decisions
Our case studies states (California, Massachusetts, Minnesota, New York, Ohio, and Wisconsin) allow self-directing program participants to have their workers work some hours that incur overtime pay liability. In addition, all of these states allow for hardship exceptions to the routine weekly limits on Medicaid billable worker hours. In all of the case study states, however, policymakers initially proposed minimizing Medicaid expenditure increases related to the FLSA's overtime pay requirements by imposing a 40-hour per week cap on individual workers' Medicaid billable hours. Advocacy on the part of self-directing program participants and their allies played a major role in convincing policymakers to not limit worker hours.
In all six of the case study states, advocacy involved coalitions of advocacy groups. These included labor unions representing participant-directed independent providers in the three states (California, Massachusetts, and Minnesota) where these workers are unionized. In Ohio, Disability Rights Ohio and ten other groups submitted comments objecting to Ohio's original proposal for a 40 hour per week "hard cap" on individual worker hours, with very limited exceptions. The policy ultimately adopted allows participant-directed workers to work up to 60 hours per week (i.e., 20 hours overtime pay) without having to apply for and gain a case manager's approval of a hardship exception. The revised policy also provides for more flexible hardship exceptions than those earlier envisioned beyond the 60 hour per week routine limit on worker hours.
Hardship Exceptions Allow Additional Worker Overtime Hours Beyond Routine Limits
Four of our case study states that have set explicit statewide program caps on participant-directed workers' billable hours (California, Massachusetts, Ohio, and Wisconsin) provide clearly defined hardship exceptions. Hardship exceptions mitigate the risk that self-directing Medicaid beneficiaries, especially those with severe disabilities, are unable to obtain workers to provide all of their authorized aide hours because all available workers are already working up to the routine limit on their Medicaid billable hours. California, in particular, offers several hardship exceptions (previously described) that permit additional overtime hours above routine limits that are already more generous than those in other states. One exception is for live-in family providers who provide services to more than one IHSS recipients, all of whom reside in the shared household. Another exception is for exceptional circumstances such as providers who are serving multiple recipients who have complex medical conditions or other special needs, reside in rural areas where other providers are not available, or need a provider who speaks their language and such providers are not otherwise available. The third exception is for service users with especially high needs who are eligible for other Medicaid benefits that allow them to receive personal care hours above the IHSS coverage limit (360 hours per month rather than the IHSS limit of 283 hours) and no other providers are available. According to the most recent statistics (2018) 2,178 hardship exceptions to the worker hours limits had been authorized.[7]
Health and Safety of Program Participants Affected Implementation Decisions
According to site visit respondents, Wisconsin's IRIS program, a 40-hour work week is viewed as preferable for the health and safety of both self-directing program participants and their workers. However, in recognition of worker shortages, permission to employ a single worker for up to 60 hours per week is readily granted. Some exceptions, primarily for live-in workers, allowing some workers to work more than 60 hours per week are also available but are less frequently approved and more likely to be time-limited.
Capping Worker Hours at the Recipient's Authorized Hours
The great majority of independent providers in California provide services to only one recipient.[10] Approximately 70 percent are family members, about half of whom reside with their service recipient.[10] Almost all live-in IHSS workers are family members. IHSS recipients sharing a household with their paid providers are typically "high need" recipients authorized to receive more than 40 hours of aide service per week. Because California is a joint employer, the live-in exemption to the FLSA overtime pay requirement is not available.[11]
The cap on worker hours imposed after the Home Care Rule went into effect in California mirrors the IHSS coverage limit for individual program participants. Based on a 30-day month, the maximum number of hours a provider may work per week is 66 -- the standard 40 plus 26 of overtime. Home care workers employed by just one consumer can work up to the consumer's maximum hours divided by 4, or 70.75 hours. The intent is to allow a provider serving a single recipient to work all of the hours authorized for an individual recipient in each month if that recipient is authorized for the 283-hour maximum program limit. As a result, self-directing program participants who have been relying on a single paid worker did not have to recruit additional providers to be able to obtain all of their authorized service hours after the Home Care Rule went into effect.
Adequacy of Managed Care Capitation Payments
Two of our case study states mandate enrollment into managed care plans. For example, since 2005 Minnesota has required all Medicaid recipients aged 65 and older to enroll in and receive all of their home and community-based long-term care services through managed care plans. Since 2013, New York requires almost all Medicaid long-term care services recipients to enroll in managed care plans.
Minnesota and New York have somewhat different relationships with their capitated managed care plans.[12] Minnesota retains more state control and delegates less decision-making authority to the plans. In addition, in New York, self-directing program participants exercise only employer authority. Although AwC FMS providers share employer authority with self-directing program participants; the AwCs all receive the same standard hourly rate for aide services. Thus, they cannot afford to authorize aide hours subject to overtime pay liability unless the managed care plans authorize them to do so and increase reimbursement in such cases accordingly. New York appropriated additional funding for managed care plan capitation payments intended to cover the costs of providing some overtime pay to providers of "high need" Medicaid beneficiaries to ensure their access to providers and promote CoC. State officials consider the managed care capitation payments to be adequately risk-adjusted.
However, Independence Care Systems (ICS), a plan that historically had enrolled a disproportionately high share of high need Medicaid personal care services users found itself increasingly facing a shortfall of funding to cover costs and had to cease operating as a managed care plan in early 2019. ICS was one of the early managed long-term services and supports (MLTSS) pilot programs in New York City and had historically specialized in serving high need Medicaid personal care services users, including exceptionally high need individuals who were provided with generous coverage that enabled them to transition from long-stay institutional care to live in the community. Prior to the issuance of the Home Care Rule, New York Labor Law (NYLL) required overtime pay only for hours in excess of 48 per week and the overtime pay required was time and a half of the state minimum wage rather than time and a half of the higher hourly rate Medicaid paid for hours not requiring overtime pay. From the ICS perspective, it was necessary to pay overtime for the workers of high need plan enrollees in order to protect those workers from loss of pay and ensure plan members' continuity of access to reliable, skilled workers. ICS saw these Home Care Rule overtime costs as not the only, but among the factors, that ultimately required ICS to cease operating as a MLTSS plan.
Ensuring adequate funding for overtime payments to ensure that high quality care and CoC from reliable workers is available to high need individuals assessed as needing more (often much more) than 40 hours of personal care aide services per week is more complicated when a state has switched from a FFS provider payments to MLTSS. The state pays MLTSS managed care organizations (MCOs) capitation payments per plan enrollee. The MCOs, in turn, are responsible for payments owed to participant-directed personal care aides, including any overtime wages. If the capitation payments the MCO received do not fully cover the cost of personal care services for high need plan members, which may include the cost of paying overtime, the MCOs will run deficits that cannot be sustained over the long-term. Kaye (2017) studied the varied approaches used to set capitation rates.[13] Among his report's concluding recommendations is the need to ensure that the rates ensure that high needs LTSS users are appropriately served:
There is a vast range of expenditures needed to meet the needs of LTSS users with different types of disabilities and different levels of need. Because high needs LTSS users are typically at greatest risk of institutional placement, states expecting plans to offer HCBS that are robust enough to reduce institutionalization must make meeting the needs of such members paramount. However, paying MCOs the same rate for all members receiving LTSS, or for all "nursing-home certifiable" members, seems likely to encourage MCOs to either deny access to needed HCBS to the highest-cost members or to find ways of excluding such individuals from participation in the plan. If a single rate is used, then it should at least be calculated based on the "case mix," using factors (aside from setting) related to the extent and type of needed services that can predict expenditures for each member.
New York has been praised for leveraging functional assessment data to risk-adjust MLTSS capitation payments.[14] New York's approach recognizes that high need individuals' services cost more (especially if they are self-directing and need to pay overtime to access CoC from aides who can meet their needs which often involve performance of routine skilled tasks). However, New York's capitation payments are risk-adjusted across the entire population of MLTSS enrollees, which tacitly assumes that people with different levels of need are evenly distributed across participating plans. In reality, some plans may attract disproportionately high need Medicaid beneficiaries compared to others because they have gained a reputation for excellence among people with disabilities who have unusually high needs that often include requiring reliable workers with paraprofessional skills who are in short supply.
In Minnesota, some self-directing program participants exercise only employer authority whereas others exercise budget authority. Minnesota has delegated authority to approve overtime hours for participant-directed home care workers who exercise employer authority to AwC FMS providers. However, the legislature did not appropriate the full amount of funding that the Governor requested to cover additional overtime pay anticipated as likely to be necessary after the Home Care Rule went into effect.
Uncertainty Concerning Joint Employment
California is the only state where a court ruling designated that state as a joint employer for aides providing services to self-directing program participants.[15] Program administration changes that Massachusetts, Oregon, and Washington have made in response to the Home Care Rule indicate those states' acceptance of joint employer status. In contrast, according to information provided by state officials during the case study research, Minnesota conducted a legal analysis and concluded that the state is not a joint employer.[16] Among the salient factors: Minnesota allows self-directing program participants to exercise budget authority. Although participant-directed workers are unionized, the collectively bargained hourly wage rate sets the wage floor and self-directing program participants may decide how many hours of aide service to purchase and may pay more per hour than the union rate if they are able to do so without over spending their budgets.
In New York, the role of AwC FMS providers and/or managed care plans as joint employers is not clear. In January 2019, a federal district court for Western New York found an AwC providing FMS for New York's Consumer Directed Personal Assistance Program (CDPAP) to be a joint employer, but this ruling by a trial level court is not a binding precedent.[17] However, if ultimately determined to be joint employers, AwCs would presumably only have those responsibilities for workers providing services to self-directing program participants who have selected that particular AwC as their FMS provider rather than one of their competitors. The same would be true of managed care plans. Thus, whether or not a particular worker working for more than one self-directing Medicaid beneficiary would be eligible for overtime pay based on aggregated hours or payment of travel time would depend on whether or not the self-directing Medicaid beneficiaries were enrolled in the same or different managed care plans and/or whether they elected to receive FMS from the same or different AwCs.
STUDY LIMITATIONS
In collecting data for the environmental scan, we did not interview representatives in all states. State decisions related to implementation of the Home Care Rule were inferred from available state documentation. However, this information was supplemented by our subcontractors (NASUAD, NASDDDS, and Applied Self Direction) direct state contacts. While there are more than 200 programs across the country that offer self-direction, we found information for fewer than 75. The findings presented here are therefore based on a subset of programs and could differ from an analysis using the entire universe of consumer directed programs. However, because the largest self-direction programs in each state are included in our database, we have collected enough data to make inferences with a moderate degree of confidence, though we recognize that these inferences may need to be revised as more data become available. Additionally, some states in our database contained multiple program entries. In states with multiple programs but consistent implementation policies, we included a single entry in the dataset. In states where multiple programs made different implementation choices, we relied on data from the program with the most extensive information.
Some states may have already chosen to limit all or some workers' Medicaid billable hours to 40 per week prior to the issuance of the Home Care Rule. We are only aware of one state (Tennessee) that had already capped all participant-directed independent providers' hours at 40 per week before the FLSA rule was promulgated. It is possible that some other states prohibited independent provider aides from working more than 40 hours per week to avoid Medicaid costs associated with having to pay overtime rates under their state's labor laws prior to the FLSA rule. However, research conducted by ASPE staff while the Home Care Rule was under development found that in states with large self-directed services programs, state labor laws often differed from the proposed federal rule. Additionally, it was often difficult to find information from publicly available sources concerning the specifics of exceptions policies in states that set explicit limits on worker hours. What we also do not know for most states is how the exception policies are communicated to self-directing program participants and participant-directed workers. Finally, the Home Care Rule has interacted with national, local and state-specific conditions in complex ways that make it challenging to determine how the Rule in isolation from other influences affected state decision-making.
CONCLUSION
The purpose of this study was to describe and document the extent to which states have made changes to their Medicaid or other publicly-funded home care programs for seniors and individuals with disabilities to comply with the 2013 update to FLSA regulations extending minimum wage and overtime protections to most home care workers, and the effect the Rule may have had on the number of hours worked and the amount of overtime compensation paid in the home care setting. This report provides an overview of early implementation activities at the state level and perspectives from various stakeholder groups.
Assuring compliance with the extension of FLSA protections to most home care workers posed a number of opportunities and challenges for states, including: in self-directed programs, determining whether the consumer is the sole employer or there is a joint employer (such as a government agency, MCO, or other entity) which may impact the worker's right to minimum wage and overtime compensation; how to apply the protections to providers who live in a consumer's home; and how to ensure proper payment for compensable travel time and overtime hours worked.
States are motivated to contain Medicaid cost increases that could result from FLSA implementation. Medicaid beneficiaries seek to assure CoC and to guarantee their ability to access aide services sufficient to provide them with all of their authorized hours. Workers are interested in gaining -- or at least not losing -- weekly income. Various organizations, including NASDDDS, National Association of Medicaid Directors, and NASUAD, provided technical assistance to state members and tried to ensure that states understood the Rule and how to comply with it.
Stakeholders agreed that DOL's goal of extending FLSA protections to home care workers was a worthy one, and they supported the goal of expanding the home care workforce, including improving pay and working conditions to recruit more workers. Many stakeholders supported the changes to the FLSA because they felt these changes would help improve working conditions for home care workers. Other stakeholders were concerned that changes to the FLSA would increase costs of home care. Many of the concerns that stakeholders had about the implementation of the Home Care Rule have generally not come to pass.
Findings from the environmental scan reveal that most states (32 including the District of Columbia) did not set a hard cap on weekly hours worked. In some cases, advocacy on the part of self-directing program participants and their allies played a crucial role in in convincing policymakers to adopt limits that were more generous. However, 16 states did set a cap at 40 hours per week, and there were three states that we could not determine their policy. States that did not set a cap as a matter of state policy, decided on a case-by-case basis whether to authorize workers to work more than 40 hours per week or delegate such case-by-case decision-making to MLTSS plans.[18]
Seventeen states have an exceptions policy for individuals who need more hours of home care service than the state's cap on worker hours ordinarily allows; however, the information on exceptions policy is limited (e.g., we could not determine the exception policy in 24 states). Capping worker hours -- especially without robust exceptions and exemptions policies -- could lead to less coordination of care and poorer quality of care. It may also have negative effects on the home care labor force, currently struggling to recruit and retain adequate numbers of workers due to low/stagnated wages and limited or no employment benefits.
Additionally, 13 states allowed self-directing program participants exercising budget authority to authorize overtime pay if they could afford to do so without over-spending their budgets. Two of these states required budget holders to obtain prior approval to do so. Not all states allowed self-directing program participants to claim the live-in exemption to the overtime pay requirement, but 11 permitted the domestic service employee exemption.
Although some promising practices have emerged among the states we profiled as case studies, each has struggled with various aspects of implementation that they are still trying to resolve, and all have made choices that could be critiqued in one way or another. Additionally, the Home Care Rule has interacted with both national and local, and state-specific conditions in complex ways that make it challenging to determine how the Home Care Rule in isolation from other influences affected state decision-making. Nevertheless, findings from this exploratory study provide the first systematic overview of state implementation of the Home Care Rule that otherwise would not be available and may be revised as more data and information becomes available.
END NOTES
-
See https://www.medicaid.gov/Federal-Policy-Guidance/Downloads/CIB-07-03-2014.pdf.
-
Some states may have already chosen to limit all or some (e.g., paid family) workers' Medicaid billable hours to 40 per week prior to the issuance of the Home Care Rule. We are only aware of one state that had already capped all participant-directed independent providers' hours at 40 per week. It is possible that some other states prohibited all independent provider aides from working more than 40 hours per week to avoid Medicaid costs associated with having to pay overtime rates under their state's labor laws. However, research conducted by ASPE staff while the Home Care Rule was under development found that states with large self-directed services programs, state labor laws often differed from the proposed federal rule. For example, in New York and Minnesota, overtime pay was not required for personal care aides until they worked more than 48 hours per week and, in New York, the overtime rate was time and a half of the state's minimum wage. In addition, we learned from speaking with state officials in some other states that overtime pay requirements were not well enforced. Prior to issuance of the Home Care Rule, CMS had never considered the question of whether states could, under Medicaid law and regulations, limit an independent provider's Medicaid billable hours or set different limits on billable hours or hourly pay rates for family versus non-family workers. When states posed the question to CMS after the Home Care Rule was promulgated, CMS determined that under Medicaid law and regulations, states had the discretionary authority to impose limits on independent provider aides' weekly Medicaid billable hours. The purpose of the DOJ/Office of the General Counsel and the CMS guidance was to advise states not to cap worker hours at 40 unless they allowed for robust hardship exceptions regardless of whether they did so in response to the issuance of the Home Care Rule or for some other reason.
-
Olmstead v. L.C., 527 U.S. 581 (1999). See also 42 U.S.C. § 12131 et seq., 28 C.F.R. pt. 35.
-
AARP Public Policy Institute (2018), National Inventory of Self-Directed Programs for the 2017 State Long-Term Services and Supports Scorecard, http://www.appliedselfdirection.com/sites/default/files/2016%20SD%20Inventory%20Final%20Report.pdf.
-
Since the Rule permitted sole employers to claim the live-in exemption, they were able to protect workers from experiencing pay cuts that would result from a limitation on workers' Medicaid billable hours per week meant to curb overtime pay liability. Self-directing program participants exercising budget authority could lower the regular wage rate of non-live-in workers to pay overtime rates for hours requiring overtime pay. Alternatively, for non-live-in paid family aides who were providing additional hours of unpaid care, they could cut the number of paid hours so they did not work hours requiring overtime pay, but raise the hourly rate for their paid hours up to 40 per week. Their workers did not gain more pay, but they did not suffer pay cuts and Medicaid expenditures did not increase.
-
Drawing on information collected in periodic inventories of self-direction programs across the United States, there has been, between 2011 and 2016, a decrease in states using the AwC model and a corresponding increase in states' use of the F/EA model.
-
Report to the Legislature on the Impact of the Fair Labor Standards Act Overtime Rule for the In-Home Supportive Services Program (2018), http://www.cdss.ca.gov/inforesources/IHSS-New-Program-Requirements.
-
IRIS Policy Manual, https://www.dhs.wisconsin.gov/publications/p0/p00708.pdf. IRIS Policy Manual Work Instructions, https://www.dhs.wisconsin.gov/publications/p0/p00708a.pdf.
-
See http://codes.ohio.gov/oac/5123:2-9-03v1. Policies apply to self-directing program participants enrolled in the Developmental Disability HCBS Waiver. Policies governing Pre-Admission Screening System Providing Options and Resources Today (PASSPORT), the HCBS waiver program for individuals with disabilities (age 60+) are less generous. They only permit workers working for more than one self-directing program participant (up to five) to work up to 56 hours per week. This higher limit appears to be to accommodate travel time pay, which suggests that Ohio accepts joint employer responsibilities, at least with respect to participant-directed workers delivering services under the PASSPORT waiver. See also, https://aging.ohio.gov/Portals/0/PDF/ODA-DOLCompliance_Choices_CD.pdf.
-
California Department of Social Services (2018), In-Home Supportive Services Program, Report to the California State Legislature on the Impact of the Fair Labor Standards Act Overtime Rule, Final Report, https://www.cdss.ca.gov/Portals/9/Leg/Final_FLSA%20Overtime%20Report%20to%20Legislature%202018.pdf?ver=2018-10-08-154455-720.
-
1983 Bonnette decision, 9th Circuit Court of Appeals, https://casetext.com/case/bonnette-v-california-health-and-welfare-agency. California state officials recognize that this court ruling, subsequently cited in lower court rulings, would likely make it difficult for the state to claim that it is not a joint employer under the Home Care Rule. The state chose to adopt a policy on worker hours and exceptions that assumed paying overtime rates to live-in workers and the legislature voted funding to implement this policy. There remains, however, a lack of judicial consensus about how to determine joint employment. A 2017 4th Circuit ruling rejected the test applied in the Bonnette case, claiming that this case has been responsible for confusion over determinations of joint employment, and substituted a different test. http://www.employmentlawdaily.com/index.php/news/4th-circuit-adopts-new-flsa-joint-employer-test-finds-general-contractor-sub-jointly-liable-for-overtime/.
-
Under a capitated contract, a MCO receives a fixed amount of money for each member it is providing care for.
-
Kaye, H. Stephen (2017), Managed LTC Services and Supports: Using Capitation Payments to Promote Home and Community-based Services. San Francisco, CA: Center for Community Living, University of California/San Francisco, School of Nursing. https://clpc.ucsf.edu/sites/clpc.ucsf.edu/files/reports/MLTSS%20Capitation%20to%20Promote%20HCBS%2011-17.pdf.
-
Vardamon, Kristol (2018), Managed Long-Term Services and Supports: Status of State Adoption and Evolution. Chapter 3 MACPAC June 2018 Annual Report to Congress on Medicaid and CHIP. Medicaid and CHIP Payment and Access Commission (MACPAC). https://www.macpac.gov/publication/managed-long-term-services-and-supports-status-of-state-adoption-and-areas-of-program-evolution/.
-
In 1983, the Ninth Circuit Court of Appeals held that, in counties providing funds to recipients to pay their own IHSS providers, the state and counties were joint employers with recipients for purposes of the Fair Labor Standards Act of 1938 (FLSA) (29 U.S.C. § 201 et seq.) and thus liable for FLSA violations. (Bonnette vs. California Health and Welfare Agency (9th Cir. 1983) 704 F.2d 1465 (9th Cir. 1983), abrogated on other grounds, Garcia v. San Antonio Metro. Transit Auth., 469 U.S. 528 (1985).
-
Information provided to project contractor Ed Kako of Mission Analytics and Mollie Murphy of Applied Self-Direction by state official Cara Benson of the Minnesota Department of Health and Human Services as part of a case study of Minnesota's response to the Home Care Rule, 2018.
-
The U.S. District Court for the Western District of New York ruled that CDPAP fiscal intermediaries are employers of personal assistants for purposes of compliance with NYLL wage and hour requirements. The decision in Hardgers-Powell v. Angels in Your Home, LLC (http://www.leadingageny.org/?LinkServID=83649223-FF6D-4933-082BD8D81520674A) arose out of a case involving a CDPAP personal assistant who sought to bring a class action lawsuit claiming that the defendants violated the NYLL and the federal FLSA by failing to pay overtime wages at the correct rate. The lawsuit also included overtime claims brought by a personal care aide and state wage notice claims. The decision creates a new precedent governing the relationship of fiscal intermediaries with personal assistants and their legal obligations. Relying on four factors, the Court concluded that the owner of Angels in Your Home, LLC is an employer of CDPAP personal assistants:
-
The owner establishes the amount of each CDPAP personal assistant's wages.
-
He maintains personnel records for CDPAP personal assistants.
-
He identifies himself and his D/B/A as the employer of record for CDPAP personal assistants, including on NYLL wage notices, in payroll and unemployment taxes, and workers compensation and statutory disability coverage.
-
Under the statutory and regulatory scheme under which participants and fiscal intermediaries operate, "the responsibilities that would be traditionally associated with one employer are divided between the participant and fiscal intermediary, who work in tandem to control each [CDPAP personal assistant's] working conditions and to ensure the delivery of home health care services."
The Court determined that, for purposes of the NYLL, the individual owner, rather than the agency, is the employer of CDPAP aides. Although the decision is not clear on this point, it appears that "Angels in Your Home" is merely a name under which the owner does business and not a legal entity, as reported by the trade association Leading Age in https://www.leadingageny.org/providers/home-and-community-based-services/fiscal-intermediaries/fiscal-intermediaries-are-employers-federal-trial-court-rules/.
-
-
Twenty-three states offer self-directed home care services under MLTSS.
