Seventy-One Million Additional Americans Are Receiving Preventive Services Coverage Without Cost-Sharing Under The Affordable Care Act
Laura Skopec and Benjamin D. Sommers, ASPE
The Affordable Care Act ensures that most insurance plans (so-called ‘non-grandfathered’ plans) provide coverage for and eliminate cost-sharing on certain recommended preventive health services, beginning on or after September 23, 2010.[1] Based in part on guidelines from the U.S. Preventive Services Task Force, this includes services such as colonoscopy screening for colon cancer, Pap smears and mammograms for women, well-child visits, flu shots for all children and adults, and many more services.[2]
While some plans already covered these services, millions of Americans were enrolled in health plans that did not. According to the Kaiser Family Foundation’s Employer Health Benefits Survey in 2012, 41% of all workers were covered by employer-sponsored group health plans that expanded their list of covered preventive services due to the Affordable Care Act.[3] The most recent data from the Census Bureau show that 173 million Americans ages 0 to 64 are enrolled in private health coverage.[4] Putting these facts together, we estimate that approximately 71 million Americans received expanded coverage of one or more preventive services in 2011 and 2012 due to the Affordable Care Act.[5]
Using national survey data on children and adults with private insurance, we next estimated how those 71 million people are distributed across states, and across age, race, and ethnic groups. We examined the following age/gender groups, and provide here a sample of the services they are now eligible for without any cost-sharing. Note that this is not an exhaustive list of covered services and is only meant to highlight several examples.
· Children (0-17): Coverage includes regular pediatrician visits, vision and hearing screening, developmental assessments, immunizations, and screening and counseling to address obesity and help children maintain a healthy weight.
· Women (18-64): Coverage includes cancer screening such as pap smears for those ages 21 to 64, mammograms for those ages 50 to 64, and colonoscopy for those ages 50 to 64; recommended immunizations such as HPV vaccination for those ages 19 to 26, flu shots for all adults, and meningococcal and pneumococcal vaccinations for high-risk adults; healthy diet counseling and obesity screening; cholesterol and blood pressure screening; screening for sexually-transmitted infections and HIV; depression screening; and tobacco-use counseling. For plan years (in the individual market, policy years) beginning on or after August 1, 2012, additional preventive services specific to women, such as well-woman visits, screening for gestational diabetes, domestic violence screening and counseling, and prescription, FDA-approved contraception, must be covered with no cost sharing.[6]
· Men (18-64): Coverage includes recommended immunizations such as flu shots for all adults and meningococcal and pneumococcal vaccinations for high-risk adults; cancer screening including colonoscopy for adults 50 to 64; healthy diet counseling and obesity screening; cholesterol and blood pressure screening; screening for HIV; depression screening; and tobacco-use counseling.
Figure 1 presents national totals, including breakdowns by age, gender, race and ethnicity. Table 1 presents totals by state.[7]
FIGURE 1: Number of Americans Estimated to be Receiving Expanded Preventive Services Coverage
Under the Affordable Care Act (in Millions)[8]
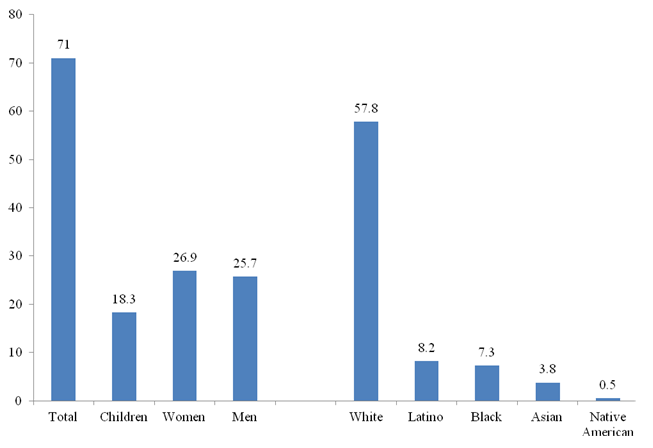
TABLE 1: Number of Americans Estimated to be Receiving Expanded Preventive Services Coverage Under the Affordable Care Act, by State
|
State |
Total |
Children |
Women |
Men |
|
Alabama |
1,084,000 |
272,000 |
426,000 |
386,000 |
|
Alaska |
164,000 |
44,000 |
60,000 |
60,000 |
|
Arizona |
1,406,000 |
377,000 |
518,000 |
511,000 |
|
Arkansas |
578,000 |
144,000 |
224,000 |
209,000 |
|
California |
8,061,000 |
2,118,000 |
2,987,000 |
2,956,000 |
|
Colorado |
1,288,000 |
348,000 |
478,000 |
462,000 |
|
Connecticut |
945,000 |
246,000 |
361,000 |
338,000 |
|
Delaware |
218,000 |
57,000 |
84,000 |
78,000 |
|
District of Columbia |
141,000 |
22,000 |
63,000 |
56,000 |
|
Florida |
3,762,000 |
912,000 |
1,470,000 |
1,380,000 |
|
Georgia |
2,202,000 |
592,000 |
843,000 |
767,000 |
|
Hawaii |
323,000 |
79,000 |
122,000 |
122,000 |
|
Idaho |
367,000 |
109,000 |
130,000 |
128,000 |
|
Illinois |
3,047,000 |
762,000 |
1,153,000 |
1,131,000 |
|
Indiana |
1,508,000 |
406,000 |
554,000 |
548,000 |
|
Iowa |
801,000 |
206,000 |
298,000 |
297,000 |
|
Kansas |
684,000 |
186,000 |
255,000 |
242,000 |
|
Kentucky |
975,000 |
243,000 |
374,000 |
359,000 |
|
Louisiana |
932,000 |
238,000 |
356,000 |
338,000 |
|
Maine |
301,000 |
70,000 |
122,000 |
109,000 |
|
Maryland |
1,518,000 |
382,000 |
590,000 |
546,000 |
|
Massachusetts |
1,773,000 |
433,000 |
690,000 |
650,000 |
|
Michigan |
2,386,000 |
637,000 |
901,000 |
848,000 |
|
Minnesota |
1,412,000 |
380,000 |
520,000 |
511,000 |
|
Mississippi |
586,000 |
152,000 |
226,000 |
208,000 |
|
Missouri |
1,441,000 |
379,000 |
532,000 |
529,000 |
|
Montana |
213,000 |
52,000 |
82,000 |
78,000 |
|
Nebraska |
477,000 |
128,000 |
176,000 |
173,000 |
|
Nevada |
615,000 |
171,000 |
223,000 |
220,000 |
|
New Hampshire |
365,000 |
91,000 |
141,000 |
133,000 |
|
New Jersey |
2,209,000 |
590,000 |
816,000 |
802,000 |
|
New Mexico |
373,000 |
95,000 |
146,000 |
132,000 |
|
New York |
4,401,000 |
1,077,000 |
1,743,000 |
1,581,000 |
|
North Carolina |
2,062,000 |
519,000 |
797,000 |
746,000 |
|
North Dakota |
180,000 |
46,000 |
67,000 |
67,000 |
|
Ohio |
2,742,000 |
695,000 |
1,037,000 |
1,010,000 |
|
Oklahoma |
811,000 |
210,000 |
309,000 |
292,000 |
|
Oregon |
907,000 |
220,000 |
360,000 |
327,000 |
|
Pennsylvania |
3,151,000 |
761,000 |
1,218,000 |
1,172,000 |
|
Rhode Island |
252,000 |
60,000 |
99,000 |
93,000 |
|
South Carolina |
980,000 |
256,000 |
388,000 |
336,000 |
|
South Dakota |
200,000 |
53,000 |
74,000 |
73,000 |
|
Tennessee |
1,413,000 |
356,000 |
542,000 |
515,000 |
|
Texas |
5,198,000 |
1,407,000 |
1,923,000 |
1,868,000 |
|
Utah |
787,000 |
267,000 |
261,000 |
259,000 |
|
Vermont |
151,000 |
31,000 |
62,000 |
58,000 |
|
Virginia |
1,998,000 |
535,000 |
765,000 |
698,000 |
|
Washington |
1,620,000 |
376,000 |
638,000 |
606,000 |
|
West Virginia |
398,000 |
96,000 |
153,000 |
148,000 |
|
Wisconsin |
1,459,000 |
378,000 |
542,000 |
538,000 |
|
Wyoming |
136,000 |
36,000 |
48,000 |
51,000 |
|
TOTAL |
71,001,000 |
18,300,000 |
26,947,000 |
25,745,000 |
[1] Interim Final Rules for Group Health Plans and Health Insurance Issuers Relating to Coverage of Preventive Services Under the Patient Protection and Affordable Care Act, U.S. Departments of Treasury; Labor; and Health and Human Services. 75 C.F.R. 41726 (Jul. 19, 2010).
[2] Recommended Preventive Services. U.S. Department of Health and Human Services, 2011. Accessed at: http://www.healthcare.gov/law/resources/regulations/prevention/recommendations.html
[3] Kaiser Family Foundation – Health Research and Education Trust. Employer Health Benefits: 2012 Summary of Findings. Exhibit 13.7 shows that 41% of workers were in plans “where the services considered preventive changed because of the ACA.” The same analysis shows that 27% of workers were in plans “where cost sharing changed for preventive services because of the ACA.” We made the conservative assumption that these two groups overlapped completely, meaning that 41% experienced expanded coverage and/or reduced cost sharing, though in fact if some people in the second group were not in the first, the overall percentage of workers affected by expanded coverage or by reduced cost sharing as a result of the ACA could have been even higher than 41% and as high as 68% (41% + 27%).
[4] DeNavas-Walt C, Proctor BD, Smith JC. Census Bureau, Current Population Reports, P60-243, Income, Poverty, and Health Insurance Coverage in the United States: 2011, Government Printing Office, Washington, DC, 2012.
[5] We included people with non-group plans in this calculation, since non-group coverage tends to be less generous than employer-provided insurance, suggesting that at least 41% of people in the non-group market likely experienced expanded coverage for preventive services due to this provision.
[6] Certain religious employers are exempt from this requirement with respect to certain contraceptive services that otherwise would be required to be covered without cost sharing. In addition, with respect to certain other non-profit organizations with religious objections to contraception coverage, the Department of Health and Human Services (and the Departments of Labor and the Treasury) have provided for a temporary enforcement safe harbor during which rulemaking is being undertaken to accommodate such objections while preserving these latter organizations’ employees’ right to contraception coverage without cost sharing.
[7] Data come from the Census Bureau’s Current Population Survey, for the years 2010-2012. We use three pooled years to allow for state-level estimates. We analyzed the proportion of all non-elderly individuals (0-64 years old) with private insurance in each category and state listed in Figure 1 and Table 1, and scaled the survey-weighted percentages to total 71 million individuals in aggregate, to match the projected number of people affected by this policy. Note that this overall approach is only a rough approximation and does not reflect any potential uneven distribution of individuals by age, race/ethnicity, or state of residence in private plans affected by the preventive coverage provisions of the Affordable Care Act.
[8] The Census Bureau records race and ethnicity separately, which means that totals combining racial and ethnic groups sum to more than 100%.
