Ellen Bouchery
Mathematica Policy Research
December 5, 2017
Printer Friendly Version in PDF Format (101 PDF pages)
ABSTRACT
Federal policies implemented in the last decade, including the Affordable Care Act (ACA) and the Mental Health Parity and Addiction Equity Act, have promoted insurance coverage for substance use disorders (SUDs). By providing funding for treatment services, these federal policies were intended to increase the proportion of individuals with SUDs who seek and receive evidence-based treatments. This report presents findings of a study to better understand how federal policies implemented in the past decade which promoted insurance coverage of substance use disorder treatment changed demand for treatment. In the same time period, the study looked at changes in capacity using national survey data, including new questions which were fielded with the National Survey of Substance Abuse Treatment Services on types of professionals in the field. A significant challenge still remains in increasing the demand for treatment among those with a substance use disorder or dependence, and in providing an adequate workforce.
DISCLAIMER: The opinions and views expressed in this report are those of the authors. They do not necessarily reflect the views of the Department of Health and Human Services, the contractor or any other funding organization
"ACRONYMS
The following acronyms are mentioned in this report and/or appendices.
| ACA | Affordable Care Act |
|---|---|
| BLS | Bureau of Labor Statistics |
| CL | Confidence Limit |
| CMS | HHS Centers for Medicare and Medicaid Services |
| DSM-IV-TR | Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision |
| FP | For-Profit |
| FTE | Full-Time Equivalent |
| HHS | U.S. Department of Health and Human Services |
| HIV | Human Immunodeficiency Virus |
| IAP | Innovation Accelerator Program |
| IC&RC | International Certification and Reciprocity Consortium |
| MH | Mental Health |
| MHPAEA | Mental Health Parity and Addiction Equity Act |
| N-SSATS | National Survey of Substance Abuse Treatment Services |
| NA | Not Available |
| NAADAC | National Association for Alcoholism and Drug Abuse Counselors |
| NP | Non-Profit |
| NSDUH | National Survey on Drug Use and Health |
| OES | Occupation Employment Survey |
| OTP | Opioid Treatment Program |
| SAMHSA | HHS Substance Abuse and Mental Health Services Administration |
| SUD | Substance Use Disorder |
| TEDS | Treatment Episode Data Set |
EXECUTIVE SUMMARY
Despite federal policies enacted within the last decade aimed at promoting insurance coverage for substance use disorders (SUDs), the existing SUD treatment workforce may be insufficient to accommodate the potential increase in demand for care and other factors may be contributing to stagnant treatment utilization rates. To address this concern, in September 2014, the U.S. Department of Health and Human Services (HHS) Office of the Assistant Secretary for Planning and Evaluation contracted with Mathematica Policy Research to conduct this project to assess current demand for SUD treatment and the state of provider capacity in the SUD treatment field. The key study findings on the demand for and supply of SUD treatment are summarized below.
Demand for SUD Treatment
Uninsured rate among individuals with SUD declined following ACA implementation.
The uninsured rate among individuals 12-64 with an SUD declined to 20 percent in 2014 from an average rate of 25 percent between 2009 and 2013. Most of this decline resulted from an increase in the rate of Medicaid enrollment, from 13 percent between 2009 and 2013 to 18 percent in 2014. This change added about 1 million individuals with SUDs to the Medicaid program.
Nevertheless, the rate of SUD treatment receipt did not increase substantially in the initial years following implementation of the ACA.
Despite the increase in insurance coverage among individuals with SUDs, evidence from multiple data sources indicates there has been no or only a small increase in treatment service use since the beginning of 2014.
Overall treatment use has remained constant, according to the National Survey on Drug Use and Health (NSDUH). According to aggregate estimates from the NSDUH, the number of individuals receiving any SUD treatment in the past year remained constant between 2004 and 2014, at about 4 million individuals (Figure ES.1). About 60 percent of these individuals (2.2-2.6 million individuals per year) received treatment in a specialty setting, which the HHS Substance Abuse and Mental Health Services Administration (SAMHSA) defined as any of the following types of facilities: hospitals (inpatient only), drug or alcohol rehabilitation facilities (inpatient or outpatient), or mental health centers.1 Because of methodological changes in the NSDUH survey implemented in 2015, the survey's estimate of 3.7 million and 2.3 million individuals receiving any and specialty treatment, respectively, in 2015 are not comparable to estimates from earlier years. According to NSDUH, between 2015 and 2016 there was again no significant change in the number of individuals receiving any and specialty treatment in the past year.
| FIGURE ES.1. Number of Individuals Who Received Any Treatment or Specialty Treatment, NSDUH 2004-2014 |
|---|
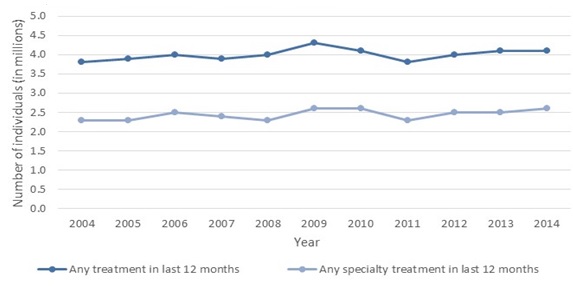 |
| SOURCE: NSDUH 2004-2014. |
National Survey of Substance Abuse Treatment Services (N-SSATS) counts of clients in treatment indicate a small increase in the number of clients in care. In contrast to the NSDUH, which measures whether a person had any treatment in the past year based on person-level responses, N-SSATS measures counts of clients in care at a point-in-time as reported by specialty SUD treatment facilities.2
N-SSATS client counts indicate a small increase in the number of clients in care between 2013 and 2015 (4.5 percent over two years), or about 56,000 individuals. About 40 percent of the growth was related to increases in inpatient hospital (which had a change of 65.6 percent) and residential care (which had a change of 11.3 percent) (Table ES.1). The increases in hospital use align with sharp increases in opioid overdoses (Rudd et al. 2016) and opioid-related admissions to intensive care units3 observed in this period. Because NSDUH excludes institutionalized individuals from its sample, N-SSATS is a more accurate source of trends in institutional service use.
The lack of change in the population with service use in the past year based on NSDUH suggests that the increase in point-in-time outpatient clients observed in N-SSATS stems from a longer duration of care. Overall, the estimated increase in SUD treatment use was minimal relative to the increases in insurance coverage and the level of unmet treatment needs.
| TABLE ES.1. Number of Clients by Setting of Care, N-SSATS 2013 and 2015 | |||
|---|---|---|---|
| Type of Care Within Setting | 2013 | 2015 | % Change |
| Total | 1,249,629 | 1,305,647 | 4.5% |
| Outpatient | 1,127,235 | 1,161,456 | 3.0% |
| Residential (non-hospital) | 107,727 | 119,900 | 11.3% |
| Hospital inpatient | 14,667 | 24,291 | 65.6% |
| SOURCE: N-SSATS 2013 and 2015. NOTE: N-SSATS surveys the universe of specialty SUD treatment facilities. In 2013 and 2015, respectively, the survey had a 94% and 92% response rate. Estimates are not adjusted for facility or item non-response. For inpatient and residential services counts indicate the number of clients in treatment on the last working day in March of each survey year. For outpatient services counts indicate the number of clients receiving services during March who are still enrolled in treatment on the last working day in March. |
|||
Lack of perceived need for treatment presents challenges in providing treatment services to those with SUDs.
Increasing treatment use for individuals with SUDs has the potential to substantially improve their welfare and that of their families as well as reduce societal and economic losses associated with SUDs, such as criminal justice costs, productivity loss, and mortality and morbidity due to accidents. The increased insurance coverage provided through recent federal policy initiatives resulted in, at most, small increases in treatment use. An important reason insurance coverage did not result in a significant expansion in treatment use is that, according to the 2015 NSDUH (Lipari et al. 2016), 95.4 percent of individuals who met criteria for an SUD but who did not receive specialty treatment (19.3 million people) did not feel they needed treatment. Among the remaining small percentage (4.6 percent, or 880,000 people) who felt they needed treatment but did not get it, 64.4 percent (about 567,000 people) reported making no effort to get treatment. Thus, expanding treatment use will require a multifaceted approach including changing attitudes about alcohol misuse and illicit drug use, increasing public awareness of treatment effectiveness, reducing stigma associated with SUD treatment, addressing financial barriers, and increasing primary care physicians' role in screening, treatment and referral.
Supply of SUD Treatment
The SUD treatment workforce comprises counselors, medical professionals, and support staff.
The 2016 N-SSATS survey found 197,559 full-time equivalent (FTE)4 paid staff and 6,726 unpaid staff in specialty SUD treatment facilities in 2016.5 About two-fifths of the FTE paid staff were counseling staff (that is, no-degree or degreed counselors); the other three-fifths were about evenly divided between medical staff (that is, physicians, nurses, pharmacists, and mid-level professionals), other support staff (that is, peer support staff, care managers, care navigators, other recovery support staff, other clinical staff and interns, pharmacy assistants, contractors/per diem staff, and intake coordinators), and administrative staff. A substantial majority of counseling staff FTEs (57 percent) had a graduate degree, but most counseling staff members with a graduate education were not certified in addiction treatment (60 percent).
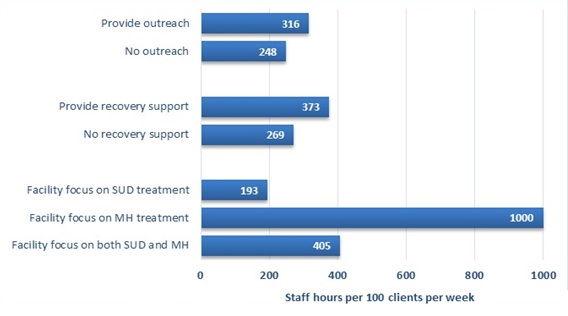
| FIGURE ES.2. Hours of Care per 100 Outpatient Clients per Week, by Facility Characteristics, N-SSATS 2016 |
|---|
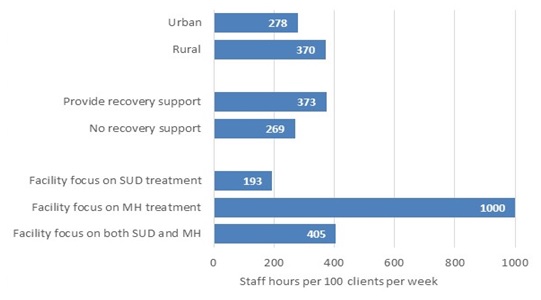 |
| SOURCE: N-SSATS 2016. NOTE: Hours of care include only non-administrative staff time. |
Outpatient treatment intensity varies based on facility characteristics.
On average, non-administrative staff provided 292 hours of care per 100 clients in outpatient treatment per week. The intensity of treatment varied substantially based on facility characteristics and services offered (Figure ES.2). Statutes and regulations for SUD treatment facilities vary by state and commonly allow facilities substantial flexibility in the professional credentials and intensity of services provided by staff (National Association of State Alcohol and Drug Abuse Directors 2013). There is little research on how staffing affects care quality.
The availability of evidence-based pharmacotherapy has increased, but challenges to further expansion remain.
Pharmacotherapy has been demonstrated to be clinically effective and cost effective for alcohol and opioid disorders (Baser et al. 2011; Mann et al. 2015). Although strong evidence suggests that the use of pharmacotherapy in managing SUDs provides substantial cost savings, the approach has not been widely adopted. The proportion of facilities offering pharmacotherapy has expanded in recent years, but still only 43 percent of facilities offered any pharmacotherapies in 2016.
| FIGURE ES.3. Staff Hours of Care per 100 Outpatient Clients per Week, by Whether Facility Provided Pharmacotherapy, N-SSATS 2016 |
|---|
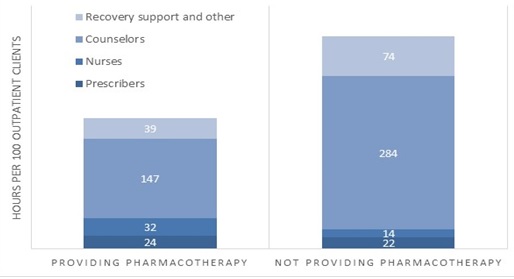 |
| SOURCE: N-SSATS 2016. NOTE: Hours of care include only non-administrative staff time. Counselors include no-degree and degreed counselors. Nurses include registered and licensed practice nurses. Prescribers include physicians and mid-level medical staff. |
Many of the barriers to expansion of pharmacotherapy are related to the workforce. The number of medical staff qualified to provide pharmacotherapy services and the staff supporting them needs to increase for provision of pharmacotherapy to expand. Training primary care providers to provide pharmacotherapy in primary care or other integrated care settings such as HIV or mental health treatment settings can improve treatment access and abstinence at six months (NIDA 2017; Korthuis et al. 2017). Primary care providers can act independently or work collaboratively with SUD treatment specialist in these models. In addition to increasing the number of qualified providers, workforce attitudes preferring behavioral therapies may need to change to attain more widespread adoption. Consistent credentialing and licensure requirements across states and insurers for professionals providing pharmacotherapy services are also needed. The HHS Opioid Strategy announced in April 2017 aims to continue the department's efforts to improve access to "treatment, and recovery services, including the full range of medication-assisted treatments" (HHS 2017); also, despite the barriers, the ACA has resulted in expansions in the number of physicians waivered to prescribe buprenorphine (Knudsen et al. 2015).
There were substantial differences in staffing patterns for outpatient treatment based on whether facilities offered pharmacotherapy (Figure ES.3). Facilities that did not offer pharmacotherapy provided nearly twice as many counselor and recovery support staff hours and about half as many nursing staff hours per 100 outpatient clients. Facilities provided a similar number of prescriber hours (including physician and mid-level medical staff) regardless of whether they provided pharmacotherapy.
Residential and inpatient hospital capacity for SUD treatment is insufficient in many states.
Despite increases in designated beds for residential and inpatient hospital SUD treatment between 2013 and 2015, utilization rates rose in these care settings. Nationally, the utilization rate for residential beds increased from 97 percent to 106 percent; that for inpatient hospital beds increased from 97 percent to 109 percent.6 In 18 states, residential bed utilization rates across all facilities were over 100 percent in 2015; the same number of states had inpatient bed utilization rates of over 100 percent.
Treatment provision at publicly operated facilities declined while care at privately operated facilities increased.
Between 2013 and 2015 clients served in public facilities declined substantially for outpatient care (13.7 percent) and somewhat for residential care (4.3 percent). Meanwhile clients served in private for-profit and private non-profit facilities expanded in these settings. This shift may be related to increased rates of insurance coverage. Inpatient clients increased substantially for facilities of all operation types.
The number of clients served in rural areas declined substantially although the population in rural areas was constant.
The number of clients receiving treatment in rural areas declined substantially (31.8 percent) and increased in urban areas (15.6 percent) between 2013 and 2015, the latest period of data available. Meanwhile, the population living in rural areas was fairly constant in this period while the population living in urban areas increased modestly (U.S. Department of Agriculture 2016). Given the treatment access barriers for individuals living in rural areas that pre-date this period, the substantial declines in treatment use in rural areas warrant further investigation.
Low wages for SUD treatment providers present challenges in expanding the workforce.
Although most SUD counselors and social workers providing SUD treatment hold post-graduate degrees, analyses of data from the Bureau of Labor Statistics show that average hourly wages for SUD treatment professionals are substantially below the average wage across all occupations and the difference between the average wage for all occupations and that for counselors has widened over the last decade, from $1.56 per hour in 2006 to $2.63 per hour in 2016. Looking at two health care professions requiring similar or fewer years of education mean hourly wages for SUD counselors were $5 and $13 lower, respectively, than those for marriage and family therapists and registered nurses.
Currently, high turnover and difficulty in hiring qualified SUD treatment staff are attributed by facility administrators to low compensation (Hyde 2013; Ryan et al. 2012; Bukach et al. 2017). Efforts to increase the supply of individuals seeking work in the SUD treatment field by increasing training program output without an associated increase in reimbursement for services or increases in funding sources are likely to result in reduced wage levels and lower retention as individuals in the SUD treatment field recognize the potential to increase their earnings by shifting to other professions.
Discussion
Policymakers at all levels of government have targeted increasing SUD treatment to address escalating drug overdose deaths related to the opioid epidemic and improve societal welfare. Meanwhile, rates of SUD treatment use generally have been constant for more than a decade despite the substantial recent increase in insurance coverage for SUD treatment. Individuals with SUD treatment needs overwhelmingly indicate that they do not feel a need for treatment and, even among the small minority who believe that they might benefit from treatment, most make no effort to obtain it. Increasing treatment penetration will require a multifaceted approach to identify and refer individuals in need to treatment, reduce treatment access barriers, and reduce stigma and change attitudes about SUDs and treatment efficacy.
Overall, the role of Medicaid in funding SUD treatment services has expanded since the beginning of 2014. There is concern that low reimbursement rates and restrictive treatment coverage under Medicaid may be a barrier to expanding treatment in some states (Dickson 2015). State Medicaid programs have the potential to play an important role in transforming the SUD treatment system and the HHS Centers for Medicare and Medicaid Services (CMS) is taking an active role encouraging states to make reforms. CMS is conducting an Innovation Accelerator Program (IAP) to support state efforts to improve care quality and continuity, enhance performance monitoring capacity, identify beneficiaries in need of treatment, develop a continuum of care that addresses the variety treatment needs and the chronic nature of SUDs, and target reimbursement models to incentivize better outcomes (CMS 2017). In addition, CMS has been working with states to improve access to and quality of SUD treatment through Medicaid Section 1115 demonstrations (CMS 2017b).
The impact of a number of recent federal efforts to increase SUD treatment use and the quality of SUD treatment services is not fully captured in the data available for this study. The initiatives include the CMS IAP as well as several SAMHSA grant programs intended to expand access to SUD treatment (McCance-Katz et al. 2017). There are also a number of federally-funded efforts to expand access to SUD screening and treatment in primary care settings and rural areas. Future years of data should be monitored to assess the impact of these initiatives.
I. INTRODUCTION
A. Purpose of Report
Despite federal policies enacted within the last decade aimed at promoting insurance coverage for substance use disorders (SUDs), the exiting SUD treatment workforce may be insufficient to accommodate the potential increase in demand for care and other factors may be contributing to stagnant treatment utilization rates. The Affordable Care Act (ACA) specifically required subsidized marketplace insurance plans, individual and small group market plans, and Medicaid expansion programs to cover SUD treatment as an essential health benefit. Two years before passage of the ACA, the 2008 Mental Health Parity and Addiction Equity Act (MHPAEA) began requiring private insurance plans that included behavioral health benefits and were offered through large group insurers to cover those services on a par with medical/surgical care (Humphreys and Frank 2014; Beronio et al. 2014).
Providing insurance coverage for SUD treatment is intended to reduce financial barriers to treatment use and thereby increase the proportion of individuals with SUD treatment needs who seek and receive evidence-based care. However, the existing SUD treatment workforce may be insufficient to accommodate an increase in demand for care and other factors may be limiting treatment utilization. To address this concern, in September 2014, the U.S. Department of Health and Human Services (HHS) Office of the Assistant Secretary for Planning and Evaluation contracted with Mathematica Policy Research to assess: (1) the current demand for SUD treatment; (2) how demand will change as more people obtain insurance coverage for this treatment; (3) the current state of capacity in the SUD treatment field; and (4) the degree to which treatment providers are prepared for integration into the broader health care system.
A previous report from this study (Bouchery et al. 2015) reviewed and analyzed the available literature and data on SUD prevalence, treatment, and workforce capacity, and incorporated information obtained through expert interviews. In the current report, we supplement the findings from the previous report with analyses of newly collected survey data on the size and characteristics of the workforce. We also reassess supply and demand trends described in the previous report, incorporating newly available data for the period following the insurance expansions that began in 2014. The following research questions guided our analyses:
1. Demand-Related Questions
-
How many people are receiving SUD treatment services, and what services are they receiving?
-
How does service receipt vary geographically?
-
What is the relationship between prevalence of SUDs and demand for care? How does this relationship vary geographically?
-
What evidence exists about how increases in Medicaid enrollment have impacted demand?
2. Supply-Related Questions
-
What are the professions and SUD treatment credentials of the current workforce?
-
What is the current capacity of service providers to supply SUD treatment services? How does provider capacity differ across geographic areas? What disparities in care access are evident (for example, by region or subpopulation)? How does provider capacity differ in relation to various services, such as inpatient, residential, intensive outpatient, outpatient, and pharmacotherapy?
-
What is the current capacity of SUD treatment organizations to participate in efforts to integrate SUD treatment within the broader health care system? To what degree are SUD treatment providers used to billing Medicaid?
-
How have wages for SUD treatment staff changed over the last decade?
B. Report Methods
We conducted the study in two phases:
-
In Phase 1, from October 2014 through December 2015, we: (1) assessed available data sources to answer the research questions and analyzed relevant data from these sources; (2) reviewed and summarized findings from the existing professional literature that addressed the questions; (3) interviewed selected experts; and (4) developed supplemental questions regarding the workforce to be fielded with an existing survey of SUD treatment facilities in 2016.
-
In Phase 2, from September 2015 through November 2017: (1) the HHS Substance Abuse and Mental Health Services Administration (SAMHSA) fielded the SUD workforce survey questions we developed, and we analyzed the results; and (2) we updated the analyses we conducted in the first phase to include newly released data so as to identify more recent trends.
Below, we briefly summarize the methods we used in conducting the study.
1. Review and Analysis of Existing Data Sources
We reviewed pre-existing sources of data regarding SUD treatment supply and demand, and identified the strengths and limitations of each. Based on this analysis, we determined which data sources were most relevant for describing the current state of and relevant trends in the supply of and demand for SUD treatment services. We obtained these data, analyzed them, and presented the results in our previous report. For the current report, we extended the analyses of selected trends for which more recent data have since become available. Appendix A provides a brief overview of the data sources analyzed in this study.
2. Literature Review
Using a defined set of key words, we searched the Cumulative Index to Nursing and Allied Health Literature, PsycINFO, Scopus, and PubMed databases for literature published from 2005 through November 2014 on the following topic areas:
-
Current demand for SUD treatment services.
-
Trends and policies impacting demand over the next decade.
-
Previous efforts to estimate the size and composition of the SUD workforce.
-
Recruiting and developing the workforce.
We also used Google to search for important studies in the gray literature. We reviewed the publication information and abstracts retrieved for relevance to our study and strength of the methodology used. We then obtained the studies most likely to provide evidence related to the four topic areas of interest and extracted relevant information from each.
3. Expert Interviews
In May and June of 2015, we interviewed three SUD workforce experts. First, we interviewed the executive director of the International Certification and Reciprocity Consortium (IC&RC), which develops standards and examinations that its local boards across the country use for credentialing and licensing. The director responded to our interview questions orally and provided written responses to the questions in our interview guide from local board staff in Louisiana, Minnesota, North Carolina, and Ohio. Next, we interviewed the executive director of the National Association for Alcoholism and Drug Abuse Counselors (NAADAC), an association for professionals in the SUD treatment workforce that also develops examinations for certifications. We conducted the third interview with the senior vice president of public policy and practice improvement for the National Council for Behavioral Health, an association of behavioral health provider organizations.
The interviews with the IC&RC and NAADAC representatives addressed trends in addiction provider certification and training programs; state requirements for licensing and certification; and recent changes in the workforce, including those associated with the ACA and MHPAEA. The interview with the National Council for Behavioral Health representative addressed the following topics:
-
Providers' experiences related to implementation of the ACA and MHPAEA.
-
How providers have adapted to the availability of expanded Medicaid and private insurance coverage for SUD treatment.
-
Barriers providers have identified related to supporting patient treatment through insurance coverage.
-
The most pressing concerns for providers related to training programs for SUD treatment professionals, recruitment and hiring of qualified staff, and retention of existing staff.
-
Those state-level differences in licensing/credentialing policies or professional certification requirements that have an important impact on the availability of SUD treatment programs or program staffing patterns.
The experts did not have data available to support responses to most questions and thus could provide only anecdotal information. They also were not able to address all topics identified. IC&RC and NAADAC representatives indicated that state board representatives might have information to address particular questions, but this information typically is not passed on to the national organization.
4. National Survey of Substance Abuse Treatment Services (N-SSATS) 2016 Supplemental Workforce Questions
Because no data had been collected on the size and composition of the SUD workforce since the late 1990s, we developed supplemental questions about them that were added to the 2016 N-SSATS, which surveys all specialty SUD treatment facilities in the United States and its territories. The supplemental questions asked facilities to identify, by profession, the total number of staff, staff hours worked in a week, and the number of paid and non-paid staff certified in addiction treatment.7
II. DEMAND FOR SUBSTANCE USE DISORDER TREATMENT
In this section, we examine recent trends in receipt of SUD treatment services by service type and geography. Then we analyze the relationship between the prevalence of SUDs and use of treatment services by type of SUD and geographic area. Last, we look specifically at the relationship between Medicaid coverage expansion and receipt of SUD treatment.
A. How Many People are Receiving SUD Treatment Services and What Services are They Receiving?
Here we analyze information on the number of people receiving SUD treatment services and the type of services they receive as derived from multiple data sources. Based on the National Survey on Drug Use and Health (NSDUH), we begin by looking at whether individuals used any services in the past year and the type of services they used. Then we analyze the number of clients in care at a given point-in-time by service type, based on the N-SSATS. Finally, we assess trends in the distribution of admissions by primary substance.
| FIGURE II.1. Number of Individuals Who Received Any Treatment or Specialty Treatment, NSDUH 2004-2014 |
|---|
 |
| SOURCE: NSDUH 2004-2014. |
1. Trends in Receipt of Any or Specialty SUD Treatment in Past Year
We use data from the NSDUH to analyze trends in SUD treatment use in the community-based population in the United States. According to the NSDUH, the number of individuals receiving any SUD treatment in the past year was relatively constant between 2004 and 2014, at about 4 million individuals (Figure II.1).
| TABLE II.1. Number of Individuals Who Received Any Treatment or Specialty Treatment, NSDUH 2015-2016 | ||
|---|---|---|
| Type of Treatment | 2015 | 2016 |
| Any treatment in past 12 months | 3.7 | 3.8 |
| Specialty treatment in past 12 months | 2.3 | 2.2 |
| SOURCE: NSDUH 2015 and 2016. | ||
About 60 percent of the individuals who received any treatment (2.2-2.6 million individuals per year) received treatment in a specialty setting, defined by SAMHSA as any of the following types of facilities: hospitals (inpatient only), drug or alcohol rehabilitation facilities (inpatient or outpatient), or mental health centers.8
Because of changes in the methodology of the survey between 2014 and 2015 survey estimates from 2015 and later may not be comparable to earlier years. Thus, we present estimates for 2015 and later separately from those in the earlier period. In 2015 there were 3.7 million and 2.3 million individuals receiving any and specialty treatment according to the NSDUH (Table II.1). Between 2015 and 2016 there was no significant change in the number of individuals receiving any and specialty treatment in the past year.
| TABLE II.2. Number of Individuals Receiving Any Specialty SUD Treatment by the Settings in Which They Received Care, NSDUH 2012-2014 | ||||||
|---|---|---|---|---|---|---|
| Type of Care | Number (in thousands) | Percentage | ||||
| 2012 | 2013 | 2014 | 2012 | 2013 | 2014 | |
| Total | 2,496 | 2,466 | 2,606 | 100 | 100 | 100 |
| Specialty settings | ||||||
| Hospital inpatient | 861 | 879 | 921 | 34 | 36 | 35 |
| Rehabilitation facility--inpatient | 1,010 | 1,042 | 1,076 | 40 | 42 | 41 |
| Rehabilitation facility--outpatient | 1,505 | 1,753 | 1,731 | 60 | 71 | 66 |
| Mental health center--outpatient | 1,000 | 1,176 | 1,157 | 40 | 48 | 44 |
| Non-specialty setting | ||||||
| Emergency room | 557 | 574 | 499 | 22 | 23 | 19 |
| Private doctor's office | 470 | 522 | 561 | 19 | 21 | 22 |
| Self-help group | 1,461 | 1,505 | 1,554 | 59 | 61 | 60 |
| Prison or jaila | 340 | 189 | 280 | 14 | 8 | 11 |
| SOURCE: NSDUH 2012-2014. NOTE: The counts only include individuals who received care in a specialty setting during the year; however, the counts indicate the number of these individuals receiving care in non-specialty settings. Counts do not sum to the total and percentages do not sum to 100% because individuals may receive care in multiple settings.
|
||||||
The distribution of the number of people receiving treatment by treatment setting also remained relatively constant from 2012 to 2014 (Table II.2) and 2015 to 2016 (Table II.3). Outpatient rehabilitation and self-help groups were the most common settings of care. About one-third of individuals who received specialty treatment received some services in an inpatient hospital; about 20 percent received emergency room care.
| TABLE II.3. Number of Individuals Receiving Any Specialty SUD Treatment by the Settings in Which They Received Care, NSDUH 2015-2016 | ||||
|---|---|---|---|---|
| Type of Care | Number (in thousands) | Percentage | ||
| 2015 | 2016 | 2015 | 2016 | |
| Total | 2,346 | 2,229 | 100 | 100 |
| Specialty settings | ||||
| Hospital inpatient | 702 | 732 | 30 | 33 |
| Rehabilitation facility--inpatient | 974 | 918 | 42 | 41 |
| Rehabilitation facility--outpatient | 1,524 | 1,446 | 65 | 65 |
| Mental health center--outpatient | 1,093 | 1,054 | 47 | 47 |
| Non-specialty setting | ||||
| Emergency room | 429 | 489 | 18 | 22 |
| Private doctor's office | 445 | 540 | 19 | 24 |
| Self-help group | 1,389 | 1,183 | 59 | 53 |
| Prison or jaila | 221 | 202 | 9 | 9 |
| SOURCE: NSDUH 2015-2016. NOTE: The counts only include individuals who received care in a specialty setting during the year; however, the counts indicate the number of these individuals receiving care in non-specialty settings. Counts do not sum to the total and percentages do not sum to 100% because individuals may receive care in multiple settings. The 2015 and 2016 estimates are not comparable to estimates from prior years due to methodological changes in the survey.
|
||||
2. Trends in Point-in-Time Clients in Care, by Care Setting
In contrast to the consistency of NSDUH findings, analysis of N-SSATS indicates notable shifts between 2013 and 2015 in client counts and the distribution of clients by service type (Table II.4).9 Overall, N-SSATS client counts indicate a small increase in clients in care between 2013 and 2015 (4.5 percent). This increase was driven by large increases in several service types: outpatient pharmacotherapy for opioid use disorders (14.8 percent), residential detoxification (34.2 percent) and short-term care (34.8 percent), and hospital inpatient detoxification (114.9 percent) and treatment (33.7 percent). There was little change in the number of clients in regular outpatient care.
The observed increases in clients receiving pharmacotherapy reflect national efforts to improve quality of care by increasing access to these evidence-based treatments. Pharmacotherapy use is associated with more consecutive weeks of abstinence from illicit opioids (Fiellin et al. 2014) and reduced mortality due to overdose (Brugal et al. 2005; Clark et al. 2011; Cousins et al. 2016; Degenhardt et al. 2009; Pierce et al. 2016) .
| TABLE II.4. Services Provided by Setting of Care, N-SSATS 2013 and 2015 | ||||||
|---|---|---|---|---|---|---|
| Type of Care | Number of Clients | Percentage of All Clients in Care | ||||
| 2013 | 2015 | % Change | 2013 | 2015 | % Change | |
| Total | 1,249,629 | 1,305,647 | 4.5% | 100.0 | 100.0 | 0.0% |
| Outpatient | 1,127,235 | 1,161,456 | 3.0% | 90.2 | 89.0 | -1.4% |
| Regular | 603,315 | 604,819 | 0.2% | 48.3 | 46.3 | -4.1% |
| Intensive | 147,162 | 128,536 | -12.7% | 11.8 | 9.8 | -16.4% |
| Detoxification | 13,839 | 14,457 | 4.5% | 1.1 | 1.1 | 0.0% |
| Day treatment/partial hospitalization | 22,828 | 23,138 | 1.4% | 1.8 | 1.8 | -3.0% |
| Methadone/buprenorphine maintenance or injectable naltrexone | 340,091 | 390,506 | 14.8% | 27.2 | 29.9 | 9.9% |
| Residential (non-hospital) | 107,727 | 119,900 | 11.3% | 8.6 | 9.2 | 6.5% |
| Detoxification | 10,244 | 13,748 | 34.2% | 0.8 | 1.1 | 28.4% |
| Short-term | 27,184 | 36,651 | 34.8% | 2.2 | 2.8 | 29.0% |
| Long-term | 70,299 | 69,501 | -1.1% | 5.6 | 5.3 | -5.4% |
| Hospital inpatient | 14,667 | 24,291 | 65.6% | 1.2 | 1.9 | 58.5% |
| Detoxification | 5,768 | 12,394 | 114.9% | 0.5 | 0.9 | 105.7% |
| Treatment | 8,899 | 11,897 | 33.7% | 0.7 | 0.9 | 28.0% |
| Clients receiving methadone, buprenorphine, or injectable naltrexone treatment | 382,237 | 439,602 | 15.0% | 30.6 | 33.7 | 10.1% |
| Clients receiving methadone | 330,308 | 356,843 | 8.0% | 26.4 | 27.3 | 3.4% |
| Clients receiving buprenorphine | 48,148 | 75,724 | 57.3% | 3.9 | 5.8 | 50.5% |
| Clients receiving injectable naltrexone | 3,781 | 7,035 | 86.1% | 0.3 | 0.5 | 78.1% |
| SOURCE: N-SSATS 2013 and 2015. NOTE: N-SSATS surveys the universe of specialty SUD treatment facilities. In 2013 and 2015, respectively, the survey had a 94% and 92% response rate. Estimates are not adjusted for facility or item non-response. For inpatient and residential services counts indicate the number of clients in treatment on the last working day in March of each survey year. For outpatient services counts indicate the number of clients receiving services during March who are still enrolled in treatment on the last working day in March. Care categories defined to align with the American Society of Addiction Medicine levels of care. |
||||||
Discrepancies between trends in the N-SSATS and NSDUH are expected due to differences in the scope of the surveys and measures of service use (Batts et al. 2014). Although both NSDUH and N-SSATS collect information on the number of individuals in care at specialty SUD treatment facilities, they differ in how they measure this population. The NSDUH measures the number of individuals reporting any receipt of treatment in the past year in a specialty setting, whereas for N-SSATS specialty facilities report the number of clients in treatment on a single day in each year (the last working day in March of each survey year). Outpatient client counts in N-SSATS include individuals receiving services during March who are still enrolled in treatment on the last working day in March. If individuals experience a longer duration of care or repeat admissions to the same type of care, NSDUH will show no change in the number of individuals with service use; N-SSATS client counts, on the other hand, will increase under these circumstances. The lack of change in the population with service use in the past year in NSDUH, paired with the increases in client counts observed in the N-SSATS, suggests that the increase in outpatient clients observed in N-SSATS stems from a longer duration of care or repeated admissions rather an increase in the total number of individuals receiving treatment in the course of a year. Analysis of the distribution of length of stay in the Treatment Episode Data Set (TEDS) Discharge file in 2012 relative to 2014 (Table II.5) supports a small 2 percentage point decline in the number of discharges with length of stay 30 days or less and corresponding 2 percentage point increase stays greater than 180 days.
| TABLE II.5. Distribution of Discharges by Length of Stay, TEDS 2012 and 2014 | ||
|---|---|---|
| Length of Stay | 2012 | 2014 |
| 1 to 30 days | 47.8 | 45.9 |
| 31 to 45 days | 6.8 | 6.7 |
| 46 to 60 days | 5.3 | 5.3 |
| 61 to 90 days | 9.0 | 9.0 |
| 91 to 120 days | 7.4 | 7.5 |
| 121 to 180 days | 8.9 | 9.2 |
| 181 to 365 days | 9.8 | 10.5 |
| More than a year | 4.9 | 6.0 |
| SOURCE: TEDS 2012 and 2014 (CBHSQ 2017a and 2017b). NOTE: Individual states report discharges to SUD treatment facilities within their state to TEDS. The scope of SUD treatment providers included in each state's data may vary over time and based on differences across states in state licensure, certification, accreditation, and disbursement of public funds. At a minimum, facilities receiving federal substance abuse treatment block grant funds are included. The following states did not report usable data for the year 2012: Kansas, Mississippi, and New Mexico. The following states did not report usable data for the year 2014: Mississippi, Florida, Georgia, Kansas, West Virginia, and New Mexico. |
||
Differences in the scope of the two surveys can explain why the N-SSATS reports show increases in residential and hospital inpatient care, whereas the NSDUH results show constant use of these services. NSDUH surveys residents in households with a fixed address and individuals in non-institutional group quarters. It excludes individuals who are institutionalized or homeless and not in a shelter from its respondent pool. Thus, the NSDUH will not accurately assess the number of individuals receiving institutional services. Specifically, NSDUH will not count hospital services provided to individuals who enter a hospital but who do not re-enter the community due to drug overdose death. Thus, N-SSATS is a more accurate source of trends in institutional service use.
3. Trends in the Primary Substance for Treatment Admission
According to the data collected in TEDS, over the last decade the primary substance for which individuals receive SUD treatment has shifted. Alcohol use disorders as a primary substance accounted for the highest proportion of clients in care in 2004 (40 percent) and 2014 (36 percent), but the proportion represented by these admissions has declined (Table II.6). The proportion of admissions for a disorder related to cocaine as a primary substance also has declined, from 14 percent to 5 percent. In contrast, the proportion of admissions for heroin and non-heroin opiates and synthetics as a primary substance rose from 18 percent to 30 percent.
| TABLE II.6. Number and Percentage of Specialty SUD Treatment Admissions by Primary Substance, TEDS 2004 and 2014 | ||||
|---|---|---|---|---|
| Number | Percentage | |||
| 2004 | 2014 | 2004 | 2014 | |
| Total | 1,808,469 | 1,614,358 | 100 | 100 |
| Alcohol | 729,366 | 585,024 | 40 | 36 |
| Marijuana | 285,193 | 247,461 | 16 | 15 |
| Heroin | 262,518 | 357,293 | 15 | 22 |
| Cocaine | 248,492 | 87,510 | 14 | 5 |
| Methamphetamine/amphetamine | 142,510 | 143,659 | 8 | 9 |
| Non-heroin opiates/synthetic | 62,895 | 134,401 | 3 | 8 |
| Other or not reported | 77,495 | 59,010 | 4 | 4 |
| SOURCE: TEDS 2004 and 2014 (SAMHSA 2016). NOTE: Individual states report admissions to SUD treatment facilities within their state to TEDS. The scope of SUD treatment providers included in each state's data may vary over time and based on differences across states in state licensure, certification, accreditation, and disbursement of public funds. At a minimum, facilities receiving federal substance abuse treatment block grant funds are included. Alaska, Arkansas, and District of Columbia reported either no data, or less than a full calendar year of data for 2004. South Carolina did not report usable data for the year 2014. |
||||
B. How Does Service Receipt Vary Geographically, by Level of Urbanicity and by Facility Operation?
Geographically. SUD prevalence and treatment use varies based on geography. Geographic variation results from cultural and environmental influences on disorder prevalence as well as differences in jurisdictional policies, treatment funding and availability, and availability of other social services. Below, we discuss the geographic variations in service receipt, reflected in Table B.1 through Table B.4.b of Appendix B.
National and regional average changes in clients by type of care between 2013 and 2015 mask substantial variation by state. Across all regions, there was a substantial increase in clients in inpatient care (65.6 percent). We also observed substantial increases for each of the four regions (Table B.1), but the increase in the Midwest was much lower than for the other regions (16.8 percent). Within each region, however, changes in inpatient care varied substantially by state (Table B.2). Residential clients increased by 11.3 percent nationally but, as was true for inpatient care, results varied by region. At the extremes, the number of residential clients in the Midwest declined by 9.6 percent, whereas the number in the South increased by 28.5 percent. Outpatient client counts increased modestly in each region.
Use of pharmacotherapies targeted to alcohol and opioid dependence substantially increased in all regions (Table B.3.a and Table B.3.b). Buprenorphine and injectable naltrexone had higher percentage increases, but these medications were less commonly used in 2013 than methadone. Rates of change varied dramatically across states, with some states seeing declines in pharmacotherapy use (particularly for methadone), whereas others saw a surge in use (Table B.4.a and Table B.4.b).
Urbanicity. Variation in treatment use based on the level of urbanicity may be expected due to access barriers for individuals in more rural areas. Jackson and Shannon (2012) reviewed the literature on barriers to treatment access for rural residents and found: (1) rural residents are less likely to have access to health insurance; (2) there is a shortage of providers in rural areas; and (3) people in need of treatment in rural areas must travel longer distances to facilities. Cummings and colleagues (2014) used the 2009 N-SSATS and the Area Resource File to look at access to outpatient SUD treatment for Medicaid enrollees. This study found that rural counties are less likely than urban counties to have at least one outpatient SUD facility that accepts Medicaid. Lenardson and Gale (2007) compared SUD treatment offered in rural and urban counties using variables in the 2004 N-SSATS. Comparing the number of facilities and treatment beds to population size revealed that rural areas actually had a larger number of treatment facilities, but the facilities had fewer inpatients beds available per population. In addition, few facilities in rural counties not adjacent to a metropolitan area provided detoxification, transitional housing services, or intensive outpatient care. Nearly all opioid treatment programs (OTPs) were located in urban areas.
| FIGURE II.2. Number of Clients by Urbanicity, N-SSATS 2013 and 2015 |
|---|
 |
| SOURCE: N-SSATS 2013 and 2015. NOTE: Pharmacotherapy is limited to methadone, buprenorphine or injectable naltrexone. Urbanicity is assigned based on the HHS National Center for Health Statistics urbanicity classification scheme. Facilities in rural areas include those in micropolitan areas with an urban core population of at least 10,000 but less than 50,000, as well as those in non-core areas. Facilities in a central or fringe urban core with a population of 50,000 or more are considered urban. Information on urbanicity was not available for all facilities; urban and rural client counts are only reported for facilities with known urbanicity. |
The number of clients in each care setting declined substantially in rural areas and increased in urban areas between 2013 and 2015 (Figure II.2). The number of clients receiving pharmacotherapy also declined substantially in rural areas and increased in urban areas with the exception of clients receiving buprenorphine which stayed fairly constant in rural areas (Table B.3.a). According to the U.S. Department of Agriculture (2016) the population living in rural areas was fairly constant in this period while the population living in urban areas has increased steadily at approximately 1 percent annually. Given the treatment access barriers for individuals living in rural areas that pre-date this period and the consistent size of the population in these areas the substantial declines in treatment use in rural areas warrant further investigation.
Facility operation. Facility operation may affect the characteristics of clients served and types of services offered as facilities that are publicly owned or non-profits may have distinct missions to provide charitable care or act as the provider of last resort. Between 2013 and 2015 clients served in public facilities (Table B.1) declined substantially for outpatient care (13.7 percent) and somewhat for residential care (4.3 percent). Meanwhile clients served in private for-profit and private non-profit facilities expanded in these settings. This shift may be related to increased rates of insurance coverage. Inpatient clients increased substantially for facilities of all operation types.
C. What is the Relationship between the Prevalence of SUDs and Demand for Care? How Does the Relationship Vary Geographically?
According to NSDUH, the number of individuals with SUDs was relatively constant between 2004 and 2014 (Figure II.3). The aggregate estimates, however, mask substantial shifts in the substances with which the disorders are associated (Table B.5). Cocaine/crack-related, hallucinogen-related, inhalant-related, and alcohol-related disorders have declined over the last decade, whereas heroin, non-medical use of psychotherapeutics, and use of pain relievers have increased.
The direction of trends in the percent of the population with use disorders was similar across age groups (Table II.7). Between 2002 and 2015, the proportion of the population with an SUD declined for all age groups for alcohol and cocaine and increased for heroin. In contrast, the proportion of the population with marijuana use disorders remained constant among individuals 26 and older, but declined for individuals 12-17 and 18-25. Due to the survey sample size and prevalence of disorders, it is difficult to detect trends in disorder prevalence among more detailed subgroups within the 26 and older group with a single year of NSDUH data. Han et al. (2017) pooled two years of NSDUH data to compare the proportion of individuals 50 and older with alcohol use disorders in 2005-2006 to 2013-2014. In contrast to the results for the 26 or older group, they found the proportion of individuals 50 and older with an alcohol use disorder increased from 3.0 percent to 3.7 percent (a 23.3 percent increase). There is concern that SUD prevalence may increase among older age groups over time as the baby boomers age given their higher rates of substance use relative to previous generations (Elinson 2015).
| FIGURE II.3. Number of Individuals Age 12 and Older with Abuse of or Dependence on Alcohol or Illicit Drugs in the Past Year, NSDUH 202-2014 |
|---|
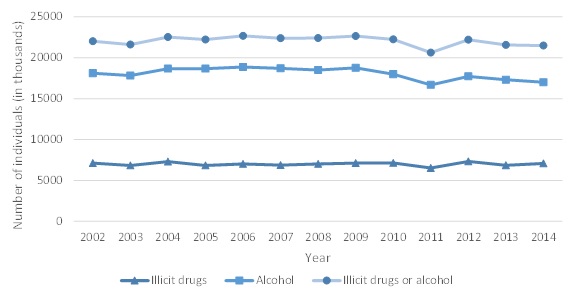 |
| SOURCE: NSDUH 2002-2014. |
According to the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition ("DSM-IV-TR" 2017), which was used to develop the diagnostic criteria in the NSDUH for having an SUD an individual must have serious negative consequences to qualify as having a disorder. For substance use dependence an individual must have three or more symptoms of dependence such as withdrawal symptoms, increased tolerance, repeated unsuccessful attempts to quit, having given up social, occupational or recreational activities or using the substance in larger amounts and for longer periods of time than intended. For abuse the individual must continue use despite having at least one negative consequence due to use including failure to fulfill a major work, school or home role, recurrent use in hazardous situations, recurrent legal issues, or social and interpersonal problems caused by use. Individuals meeting criteria for a disorder continue substance use despite serious negative consequences in their personal lives.
| TABLE II.7. Percentage of Population with an SUD by Type of Substance and Age Group, NSDUH 2002 and 2015 | ||||||
|---|---|---|---|---|---|---|
| Age 12-17 | Age 18-25 | Age 26 or Older | ||||
| 2002 | 2015 | 2002 | 2015 | 2002 | 2015 | |
| Alcohol use | 5.9* | 2.5 | 17.7* | 10.9 | 6.2* | 5.4 |
| Marijuana use | 4.3* | 2.6 | 6.0* | 5.1 | 0.8 | 0.8 |
| Cocaine use | 0.4* | 0.1 | 1.2* | 0.7 | 0.6* | 0.3 |
| Heroin use | 0.1 | 0.0 | 0.2* | 0.4 | 0.1* | 0.2 |
| SOURCE: NSDUH 2002 and 2015 (CBHSQ 2016b). * Estimate is significantly different from 2015 estimate at the 0.5% level. |
||||||
Based on the NSDUH survey, there is a substantial gap between the number of people with an SUD and the number of individuals who receive specialty treatment in a given year. In 2014, an estimated 20.3 million United States residents aged 12-64 met criteria for an SUD in the past year. Among this group, less than 10 percent of individuals abusing or dependent on alcohol only received specialty SUD treatment in the past year (Figure II.4). The treatment rate was higher (about 20 percent) among individuals abusing or dependent on illicit drugs only. About 15 percent of those abusing or dependent on both illicit drugs and alcohol received treatment. Differences between the 2013 and 2014 rates are not statistically significant. According to a review by Foster (2014), treatment rates among individuals with SUDs are substantially lower than those for common health conditions, such as hypertension (77 percent), diabetes (73 percent), and major depression (71 percent). However, an individual's need for professional support to address an SUD may depend on several factors, such as the severity of the disorder, comorbid health conditions, personal coping skills, the individual's environment, and available sources of informal specialty support (Mechanic 2003). Treatment rates vary little across states (Table B.6).
| FIGURE II.4. Percentage of Individuals Age 12-64 with Abuse or Dependence Who Received Specialty SUD Treatment, 2013-2014 |
|---|
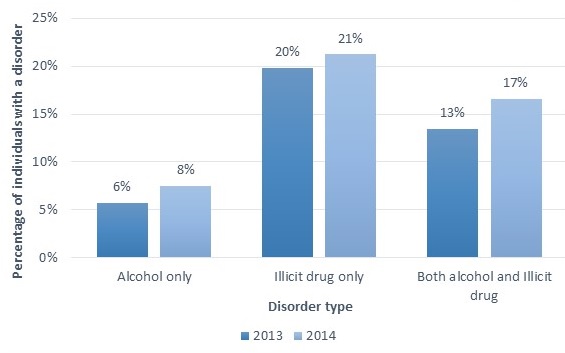 |
| SOURCE: Mathematica analysis of NSDUH 2013 and 2014 public use files. |
Individuals who meet the criteria for an SUD but do not receive treatment fall into three groups: (1) those who do not feel they need treatment; (2) those who feel they need treatment but do not seek it; and (3) those who feel they need and seek treatment but do not receive it. Based on the 2015 NSDUH, Lipari et al. (2016) found that 95.4 percent of people who met the criteria for an SUD but did not receive specialty treatment did not feel they needed treatment (19.3 million people). Among the remaining small percentage (4.6 percent, or 880,000 people) who felt they needed treatment but did not get it, 64.4 percent (about 567,000 people) reported making no effort to get treatment, whereas 35.6 percent (about 313,000 people) reported they did make such efforts. Figure II.5 displays trends in the number of individuals who received specialty SUD treatment, felt they needed treatment but did not seek it, and felt they needed treatment and sought it but did not receive it. These numbers were relatively constant from 2004 through 2014.
| FIGURE II.5. Number of Individuals Who Received Specialty SUD Treatment or Felt They Needed but Did Not Receive Treatment, NSDUH, 2004-2014 |
|---|
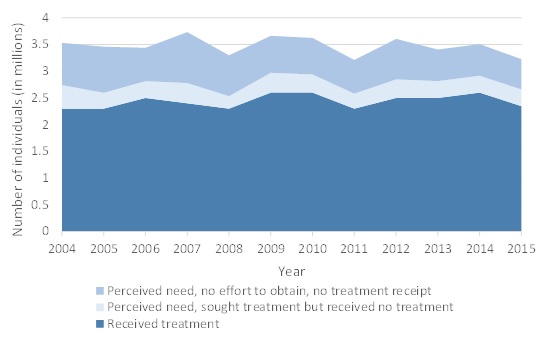 |
| SOURCE: NSDUH 2004-2014. NOTE: The figure depicts treatment receipt within the past 12 months. |
D. What Evidence Exists about How Increases in Medicaid Enrollment Have Impacted Demand?
In Phase 1 of this project we reviewed the literature on the relationship between Medicaid insurance coverage and SUD treatment use. We found only a few studies in the literature that have explicitly examined how health insurance coverage impacts demand for SUD treatment services; furthermore, many of these studies did not employ experimental designs, so the findings may be confounded by other factors. Although a rigorous study with experimental design found that insurance coverage has a positive effect on the use of general health services (Newhouse and the Insurance Experiment Group 1993), findings for SUD treatment could differ for several reasons. First, SUD treatment is typically provided outside of the general health sector, and insurance coverage for these services may be less comprehensive, have a limited network of providers, and require greater out-of-pocket costs for the client, thereby deterring treatment use. The social stigma attached to SUDs and SUD treatment may also limit treatment seeking despite insurance coverage. In addition, states and the Federal Government (through block grants) fund SUD treatment directly, particularly for those who are uninsured. Thus, although other types of care may be more affordable for those who are insured, the availability of publicly funded SUD treatment for individuals without insurance may mean that access to Medicaid coverage has less impact on SUD treatment use than use of other types of health care services.
The findings from the limited studies we identified on the relationship between Medicaid coverage and SUD treatment use indicate that individuals with Medicaid coverage are more likely to use SUD treatment than those with private insurance or who are uninsured (Bouchery et al. 2012; Epstein et al. 2004; Larson et al. 2005). This finding may be due to out-of-pocket expenses being lower under Medicaid. It may also be due to differences in the care management and benefit packages provided through Medicaid and private insurance plans. Since these studies did not use an experimental design the findings may be due to characteristics of the Medicaid population that were not controlled for in the models. In particular, individuals who are eligible for Medicaid may be enrolled in Medicaid by a treatment provider.
For Phase 2 of this study data from the NSDUH on Medicaid enrollment and treatment use prior to (2009-2013) and following ACA implementation (2014) was available for analysis. We used these data to estimate how increased rates of Medicaid enrollment influenced SUD treatment use. First, among individuals with SUDs we estimated changes in Medicaid enrollment rates and the number of individuals with SUD who gained Medicaid coverage as a result of increased enrollment rates. Then we estimated treatment use rates among those with SUDs and assessed how access to Medicaid coverage likely affected treatment use among individuals who gained Medicaid coverage.
According to our analysis of the NSDUH, the proportion of individuals ages 12-64 with SUDs who were enrolled in Medicaid rose from 13.4 percent in the five years from 2009 to 2013 to 18.1 percent in 2014--a statistically significant change (Table II.8). There was a corresponding decline in the percentage uninsured from 24.8 percent in 2009-2013 to 20.0 percent in 2014. This change may be related to expansion of Medicaid eligibility under the ACA. The opioid epidemic and efforts to increase treatment use for individuals affected may also have contributed to increased Medicaid enrollment among individuals with SUDs.
Because of the higher Medicaid enrollment rate observed in 2014, we estimate that approximately 944,000 more individuals with SUDs were enrolled in Medicaid in 2014 than would have been expected, given the Medicaid enrollment rates observed between 2009 and 2013 (Table II.9). This represents a 34 percent increase in the size of the Medicaid population with SUDs. We estimate this by projecting what Medicaid enrollment would have been among individuals with SUDs given the average enrollment rate in 2009-2013 compared to the observed enrollment rate in 2014. The steps of this calculation are presented in Table II.9. The first step was to determine the actual number of individuals enrolled in Medicaid with SUDs in 2014. Then we calculated the ratio of the observed average Medicaid enrollment rate in 2009-2013 relative to that for 2014 based on the estimates in Table II.8. We multiplied these ratios by the actual number of Medicaid enrollees with an SUD in each diagnostic category in 2014 to calculate projected Medicaid enrollment for 2014 given the average enrollment rate between 2009 and 2013. We then subtracted the projected enrollment levels for 2009-2013 from the actual enrollment levels in 2014 to estimate the increase in the number of enrollees.
| TABLE II.8. Percentage of Individuals Ages 12-64 with SUDs Who Were Enrolled in Medicaid or Uninsured in 2009-2013 versus 2014, by SUD Type | ||||||
|---|---|---|---|---|---|---|
| Type of Substance | 2009-2013 | 2014 | ||||
| Mean | Lower Bound for 95% CL |
Upper Bound for 95% CL |
Mean | Lower Bound for 95% CL |
Upper Bound for 95% CL |
|
| Medicaid Enrolled | ||||||
| Total | 13.4 | 12.8 | 14.1 | 18.1 | 16.7 | 19.6 |
| Alcohol dependence | 11.1 | 9.9 | 12.3 | 16.6 | 14.0 | 19.2 |
| Other alcohol and marijuana disorders | 11.7 | 11.0 | 12.5 | 14.9 | 13.4 | 16.4 |
| Other drug abuse or dependence disorders | 23.1 | 21.4 | 24.7 | 30.9 | 27.3 | 34.5 |
| Uninsured | ||||||
| Total | 24.8 | 23.7 | 25.9 | 20.0 | 18.3 | 21.7 |
| Alcohol dependence | 25.4 | 23.9 | 26.8 | 23.6 | 20.2 | 27.0 |
| Other alcohol and marijuana disorders | 22.7 | 21.4 | 24.0 | 17.0 | 14.9 | 19.1 |
| Other drug abuse or dependence disorders | 30.4 | 28.1 | 32.8 | 22.5 | 18.5 | 26.6 |
| SOURCE: NSDUH 2009-2014. | ||||||
| TABLE II.9. Estimated Increase in Medicaid Enrollment Associated with Medicaid Expansion for Individuals Ages 12-64 with an SUD, by SUD Type | ||||
|---|---|---|---|---|
| Type of Substance | 2014 Medicaid Enrollmenta | 2009-2013 Medicaid Enrollment Rate as a Percentage of 2014 Rateb |
Projected 2014 Medicaid Enrollment Based on 2009-2013 Enrollment Ratesc |
Estimated Increase in Medicaid Enrollment Associated with Medicaid Expansiond |
| Total | 3,684,517 | 74 | 2,740,333 | 944,184 |
| Alcohol dependence | 1,042,102 | 67 | 699,424 | 342,678 |
| Other alcohol and marijuana disorders | 1,571,584 | 79 | 1,241,446 | 330,138 |
| Other drug abuse or dependence disorders | 1,070,831 | 75 | 799,463 | 271,368 |
SOURCE: Mathematica analysis of NSDUH 2009-2014 public use files.
|
||||
According to the NSDUH, in 2014 most Medicaid-enrolled individuals with an SUD, 85 percent, did not receive any specialty treatment. Assuming their treatment use rates are similar to those of the Medicaid population overall, most of the individuals whose enrollment is associated with Medicaid expansion (about 798,000, or 85 percent of the 944,000) did not receive any specialty SUD treatment in 2014 (Figure II.6). Individuals who are uninsured access treatment at a lower rate than those on Medicaid; a logit model predicting specialty treatment use for the NSDUH using data from 2009 to 2014 indicated that the likelihood of specialty SUD treatment for someone who was uninsured was 60 percent of that for an individual who was Medicaid insured. Thus, we would expect 60 percent of those whose enrollment in Medicaid was associated with Medicaid expansion who received SUD treatment in 2014 would have received specialty SUD treatment even if they were uninsured. The remaining approximately 59,000 (40 percent) would not have received specialty treatment in the absence of Medicaid enrollment.10
| FIGURE II.6. Estimated Rate of Treatment Receipt among Medicaid Expansion Population Ages 12-64 with an SUD, 2014 |
|---|
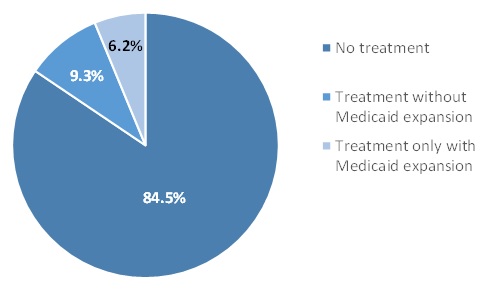 |
| SOURCE: Mathematica analysis of NSDUH 2009-2014 public use files. NOTE: We estimated the percentage receiving any specialty treatment (15.5%) based on the observed rate of specialty SUD treatment receipt in the NSDUH 2009-2014 for Medicaid-enrolled individuals ages 12-64 with an SUD. We estimated the share of individuals who would have received treatment without Medicaid expansion based on findings from a logit model using NSDUH 2009-2014 data, which indicated the likelihood of specialty treatment use for uninsured individuals was 60% of that for Medicaid-enrolled individuals. |
A limitation to this analysis is that we assume that the SUD treatment use rate for the Medicaid expansion population with SUDs is the same as that for other Medicaid enrollees with SUDs. To assess the importance of this limitation, we compared treatment use rates by disorder type in 2014 to the average for 2009-2013. Despite the 34 percent increase in the number of individuals enrolled in Medicaid with SUDs specialty treatment use rates were unchanged between the two periods suggesting that the expansion population had similar rates of treatment use.
| TABLE II.10. Percentage of Individuals Ages 12-64 with SUDs Who Were Enrolled in Medicaid Who Used Specialty Treatment in 2009-2013 versus 2014, by SUD Type | ||||||
|---|---|---|---|---|---|---|
| Type of Substance | 2009-2013 | 2014 | ||||
| Mean | Lower Bound for 95% CL |
Upper Bound for 95% CL |
Mean | Lower Bound for 95% CL |
Upper Bound for 95% CL |
|
| Total | 14.5 | 12.7 | 16.3 | 15.5 | 11.8 | 19.2 |
| Alcohol dependence | 10.7 | 7.3 | 14.0 | 11.1 | 5.5 | 16.8 |
| Other alcohol and marijuana disorders | 8.3 | 6.3 | 10.3 | 9.6 | 4.4 | 14.9 |
| Other drug abuse or dependence disorders | 28.2 | 24.2 | 32.2 | 28.2 | 20.1 | 36.4 |
| SOURCE: Mathematica analysis of NSDUH 2009-2014 public use files. | ||||||
Another limitation of this analysis is that it included only individuals with SUDs as identified by responses to questions in the NSDUH survey. Some individuals receive treatment for substance use, but do not meet criteria for an SUD in the past year. These may be individuals who previously met criteria for a disorder and are continuing to receive treatment to reduce the likelihood of relapse. According to the NSDUH, on average between 2009-2013 and in 2014, respectively, about 292,000 and 261,000 individuals enrolled in Medicaid who did not meet criteria for an SUD in the past year received specialty treatment (Table II.11). The difference between these estimates is not statistically significant suggesting the Medicaid expansion did not substantially change the number of individuals in this population receiving specialty treatment.
| TABLE II.11. Number of Individuals Ages 12-64 Not Meeting Criteria for an SUD Who Received Specialty SUD Treatment in 2009-2013 versus 2014, by Medicaid Enrollment | ||||||
|---|---|---|---|---|---|---|
| Type of Substance | 2009-2013 | 2014 | ||||
| Mean | Lower Bound for 95% CL |
Upper Bound for 95% CL |
Mean | Lower Bound for 95% CL |
Upper Bound for 95% CL |
|
| Medicaid enrolled | 291,898 | 243,132 | 340,664 | 261,103 | 179,849 | 342,356 |
| Not Medicaid enrolled | 672,861 | 588,171 | 757,551 | 728,473 | 540,615 | 916,332 |
| SOURCE: Mathematica analysis of NSDUH 2009-2014 public use files. | ||||||
III. SUPPLY OF SUBSTANCE USE DISORDER TREATMENT
In this section, we present our findings on the supply of SUD treatment services. The primary data source for these analyses is the information collected on the workforce questions added to the 2016 N-SSATS. These data are supplemented with information from the N-SSATS on trends in facility acceptance of insurance and utilization rates in beds designated for SUD treatment as well as data from Bureau of Labor Statistics (BLS) on trends in hourly wages.
A. What are the Professions and SUD Treatment Credentials of the Current Workforce?
Provision of SUD treatment requires a mix of counselors, medical professionals, and support staff. The level and type of staff needed vary across care types and settings, based on the needs of the clients in care. In this section, we present findings from recent N-SSATS 2016 survey data that characterize this multifaceted workforce, providing information on its overall size, composition, education, and training.
1. What is the Size of the SUD Treatment Workforce?
According to the N-SSATS survey, 256,449 paid staff members (representing 197,559 full-time equivalent [FTE] positions) and 14,458 unpaid staff members (representing 6,726 FTE positions) worked in specialty SUD treatment facilities in 2016 (Table B.7 and Table B.8). We define an FTE as 40 working hours per week. About two-fifths of the paid FTEs were degreed and no-degree counseling staff (Figure III.1). The other three-fifths of the paid FTEs were about evenly divided between medical staff (that is, physicians, pharmacists, nurses, and mid-level professionals), other support staff (that is, peer support staff, care managers, patient navigators, other recovery support staff, other clinical staff and interns, pharmacy assistants, contractors/per diem staff, and intake coordinators), and administrative staff.
| FIGURE III.1. Distribution of Paid FTEs by Staff Type, 2016 |
|---|
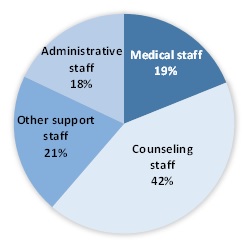 |
| SOURCE: N-SSATS 2016. NOTE: FTE is based on 40 working hours per week. |
2. What is the Education Level of Medical and Counseling Staff?
The training and educational attainment of staff in specialty SUD treatment facilities varied. There are few standards for such staffing. State and federal regulations allow SUD treatment facilities substantial flexibility in selecting the number and types of professionals they employ. Thus, facilities can align their staff with the needs of their client population and the services they offer. In this section, we provide an overview of SUD specialty facility staffing nationally, based on Table B.7. More detailed information by state and facility characteristics is provided in Appendix B (Table B.9.a, Table B.10.a, and Table B.11.a).
Physicians and other prescribers are particularly important in expanding the use of pharmacotherapy. The SAMHSA-HRSA Center for Integrated Health Solutions (2014) identified lack of available prescribers as a barrier to expanding pharmacotherapy use. Physicians accounted for 20 percent (7,576 FTEs) of the medical staff at specialty SUD treatment facilities (Figure III.2). These physicians are supplemented by 4,043 FTEs for mid-level medical personnel (including nurse practitioners, physician assistants, and advanced practice nurses) who can also prescribe. Although they make up a small share of all medical staff (3 percent), pharmacists, who accounted for 1,110 FTEs, are also important in supporting opioid treatment facilities. Nurses are the most common type of medical staff in specialty SUD treatment facilities. About two-thirds of nursing staff are registered nurses (16,515 FTEs) and one-third are licensed practical nurses (8,073 FTEs).
| FIGURE III.2. Distribution of FTE Medical Staff, by Training |
|---|
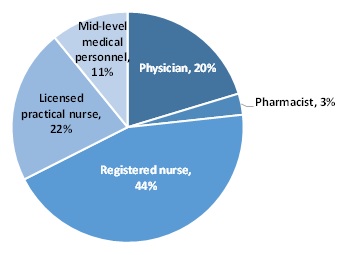 |
| SOURCE: N-SSATS 2016. NOTE: FTE is based on 40 working hours per week. |
Counseling staff in SUD treatment facilities have high rates of post-graduate education. A substantial majority (57 percent) of counselors (including degreed and no-degree counseling staff) in these facilities have a graduate degree (Figure III.3). Only 17 percent of counselors have less than a bachelor's degree.
| FIGURE III.3. Distribution of FTE Counseling Staff, by Education Level |
|---|
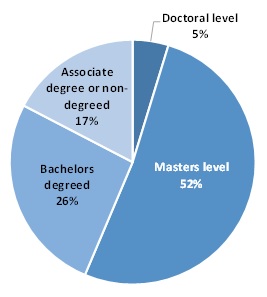 |
| SOURCE: N-SSATS 2016. NOTE: FTE is based on 40 working hours per week. |
3. What Percentage of Specialty SUD Treatment Staff are Certified in Addiction Treatment?
Although counseling staff in SUD treatment facilities have high rates of post-graduate education, this advanced education may not translate into greater knowledge specific to SUD treatment, as many graduate programs in social work and psychology do not provide specialized training in SUDs. Community colleges provide much of the specialized academic training in SUDs (McCarty 2002; Institute of Medicine 2006). Addiction counselors can demonstrate their competency by obtaining certification through organizations such as IC&RC and NAADAC. Certification is available for different levels of staff and requires education/training, work experience, and an exam focused on SUDs and addiction. Certification in addiction treatment was more common among counselors with less educational attainment. In fact, as shown in Figure III.4, only 40 percent and 34 percent of master's-level and doctoral-level counselors, respectively, are certified in addiction treatment in contrast to 49 percent and 59 percent, respectively, for bachelor's degree and associate's degree or no-degree counselors. Overall, 31 percent of non-administrative staff in specialty SUD treatment facilities are certified in addiction treatment.
This section provides an overview of staff certification in addiction at SUD specialty facilities nationally. More detailed information on certification by state and facility characteristics is provided in Appendix B (Table B.9.b, Table B.10.b, and Table B.11.b).
| FIGURE III.4. Percentage of Specialty SUD Treatment Staff Certified in Addiction Treatment, by Type of Staff |
|---|
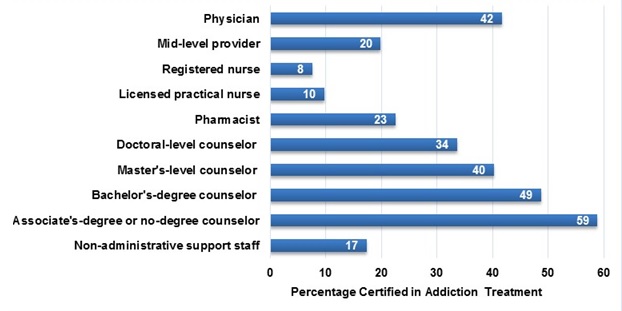 |
| SOURCE: N-SSATS 2016. NOTE: Non-administrative support staff includes pharmacy assistants, peer support staff, care managers, patient navigators, other recovery support workers, interns, contractors, per diem staff, intake coordinators, and other clinical staff not included in other groups. |
B. What is the Current Capacity of Service Providers to Supply SUD Treatment Services? How Does Provider Capacity Differ Across Geographic Areas? What Disparities in Care Access are Evident? How Does Provider Capacity Differ in Relation to Various Services, such as Inpatient, Residential, Intensive Outpatient, Outpatient, and Pharmacotherapy?
There are limited data available to assess treatment system capacity despite its importance and relevance in further policymaking. In this section, we provide information on the number of staff hours utilized per week for every 100 outpatient clients and the variation in this metric based on facility characteristics. We also provide data on access to pharmacotherapy and utilization rates for designated residential and inpatient care beds.
1. For Every 100 Clients in Outpatient Care, How Many Hours of Care are provided per Week by Type of Staff? How Does the Level of Hours provided Vary by State, Types of Services Offered, and Other Facility Characteristics?
In this section, we report staff hours per week for every 100 clients in care by type of staff and facility characteristics. We limit this analysis to facilities that provide only outpatient treatment. The level and distribution of staff hours provided differs substantially based on whether pharmacotherapies are offered at the facility. Overall, on average, for every 100 clients in care, outpatient facility staff provide 292 hours of services per week (Table III.1). Fewer staff hours were used per 100 clients in facilities providing pharmacotherapies (242 hours per week) than in those not providing pharmacotherapies (393 hours per week). In both groups, the bulk of hours were provided by counseling staff (66 percent across all facilities); however, medical staff accounted for a greater share of hours in facilities providing pharmacotherapy (25 percent) than those that did not (10 percent). Facilities providing no pharmacotherapy used substantially more counseling and recovery support staff hours than those providing pharmacotherapy. Detailed information on the level and distribution of staff hours per client per week by state are listed in Table B.12.a, Table B.12.b, and Table B.12.c.
| TABLE III.1. Staff Hours per 100 Outpatient Clients per Week, by Type of Staff and Availability of Pharmacotherapy, 2016 | ||||||
|---|---|---|---|---|---|---|
| Type of Staff | Number | Percentage | ||||
| All Facilities | Facilities Providing an Pharmaco-therapies |
Facilities Providing No Pharmaco-therapy |
All Facilities | Facilities Providing an Pharmaco-therapies |
Facilities Providing No Pharmaco-therapy |
|
| Total | 292 | 242 | 393 | 100 | 100 | 100 |
| Medical staff | 52 | 60 | 38 | 18 | 25 | 10 |
| Physician | 15 | 15 | 14 | 5 | 6 | 4 |
| Pharmacy staff | 3 | 3 | 2 | 1 | 1 | 1 |
| Mid-level medical personnel | 9 | 9 | 8 | 3 | 4 | 2 |
| Registered nurse | 14 | 15 | 10 | 5 | 6 | 2 |
| Licensed practical nurse | 13 | 17 | 4 | 4 | 7 | 1 |
| Counselors | 192 | 147 | 284 | 66 | 61 | 72 |
| Post-graduate level | 113 | 87 | 167 | 39 | 36 | 42 |
| Bachelor's degree | 51 | 39 | 75 | 17 | 16 | 19 |
| Associate's or no-degree | 27 | 20 | 42 | 9 | 8 | 11 |
| Recovery support staff | 47 | 36 | 72 | 16 | 15 | 18 |
| SOURCE: N-SSATS 2016. | ||||||
| FIGURE III.5. Staff Hours per 100 Outpatient Clients per Week, by Facility Services Offered, 2016 |
|---|
 |
| SOURCE: N-SSATS 2016. NOTE: We identified facilities as providing outreach if they said they offered outreach to persons who may need treatment (SRVC91 = 1). We identified facilities as providing recovery support services if they provided social skills development, mentoring/peer support, assistance in obtaining social services, employment counseling or training, or assistance in locating housing (SRVC96 = 1, SRVC97 = 1, SRVC36 = 1, SRVC39 = 1, and SRVC38 = 1). We determined facility focus based on responses to Question 6. |
Unsurprisingly, when we examined disparities across facilities in staff hours per 100 clients per week based on differences in services offered (Table B.13), facilities that reported providing supplemental services such as outreach to individuals in the community who may need treatment and recovery support services averaged higher staff hours per 100 clients per week (Figure III.5). Most striking were the differences based on facility primary focus. Those that reported a dual focus on mental health and substance abuse treatment (405 hours per 100 clients per week) or primarily mental health treatment (1,000 hours per 100 clients per week) reported substantially higher staff hours per 100 clients per week relative to those whose focus was primarily SUD treatment (193 hours per 100 clients per week).
| FIGURE III.6. Staff Hours per 100 Outpatient Clients per Week, by Urbanicity, Operation, and Size, 2016 |
|---|
 |
| SOURCE: N-SSATS 2016. NOTE: We assigned urbanicity based on the National Center for Health Statistics urbanicity classification scheme. Facilities in rural areas include those in micropolitan areas with an urban core of at least 10,000 but less than 50,000 population, as well as those in non-core areas. Facilities in a central or fringe urban core of 50,000 or more are considered urban. Information on urbanicity was not available for all facilities; urban and rural estimates are reported only for facilities with known urbanicity. Facility operation was self-designated in N-SSATS Question 7. We determined facility size based on the number of outpatient clients in care. We identified facilities below the 25th and above the 75th percentiles for client count as small and large, respectively. We designated the remaining facilities as medium. |
There were also substantial differences in staff hours per 100 clients per week based on facility characteristics such as urbanicity and size (Table B.14). Some of these differences may result from economies of scale achieved in larger facilities. For example, rural facilities and those with fewer clients used substantially more staff hours per 100 clients (Figure III.6). There were also substantial differences based on facility operation. These differences may be related to differences in facility mission that align with operation. Public facilities often serve as the providers of last resort and serve clients with comorbid conditions and limited social and economic supports. Thus, it is not surprising that public facilities reported the highest numbers of hours per 100 clients (432 hours per 100 clients per week) followed by non-profit facilities (339 hours per 100 clients per week).
2. What Proportion of Facilities Provide Pharmacotherapy?
Pharmacotherapy has been demonstrated to be both clinically and cost effective for alcohol and opioid disorders (Mann et al. 2014; Baser et al. 2011). Although there is strong evidence that use of pharmacotherapy in managing SUDs provides substantial cost savings, this approach is not widespread. The proportion of facilities offering any pharmacotherapy, including those related to opioid use, has expanded in recent years as efforts to improve the quality of SUD treatment have focused on promoting its use. Overall, in urban and rural areas and across all facility operation types, the percentage of facilities offering any pharmacotherapies and specifically, opioid-related pharmacotherapies, has increased modestly from 2013 to 2016 (Figure III.7 and Figure III.8). Overall, however, only 43 percent of facilities offered any pharmacotherapies in 2016.
| FIGURE III.7. Percentage of Facilities Offering Any Pharmacotherapies, 2013 and 2016 |
|---|
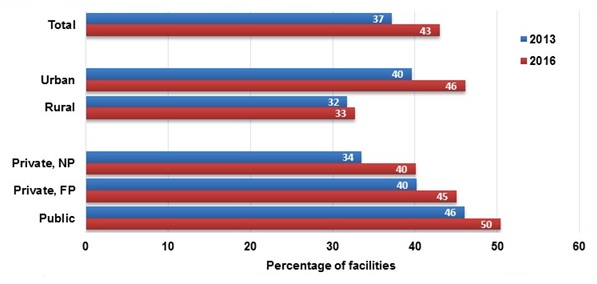 |
| SOURCE: N-SSATS 2016. NOTE: We assigned urbanicity assigned based on the National Center for Health Statistics urbanicity classification scheme. Facilities in rural areas include those in micropolitan areas with an urban core of at least 10,000 but less than 50,000 population, as well as those in non-core areas. Facilities in a central or fringe urban core of 50,000 or more are considered urban. Facility operation was self-designated in N-SSATS Question 7. |
Facility primary focus is associated with the availability of pharmacotherapies. Facilities indicating their primary focus was mental health treatment were substantially less likely to offer any pharmacotherapies (35 percent) than their counterparts focusing on SUDs (44 percent) or SUDs and mental health treatment (42 percent) (Figure III.9). This difference was more substantial when we assessed provision of pharmacotherapies for opioid-related disorders. Only 24 percent of facilities focusing on mental health treatment offered pharmacotherapy for opioid disorders. In contrast, 41 percent and 34 percent of facilities focusing on SUD treatment and SUD and mental health treatment, respectively, provided opioid-related pharmacotherapies.
| FIGURE III.8. Percentage of Facilities Offering Opioid-Related Pharmacotherapies, 2013 and 2016 |
|---|
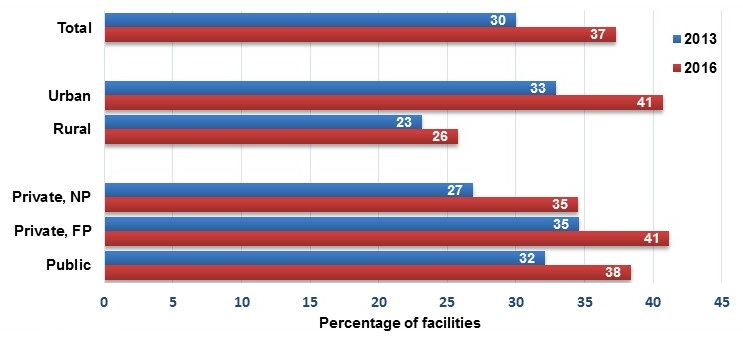 |
| SOURCE: N-SSATS 2016. NOTE: We assigned urbanicity based on the National Center for Health Statistics urbanicity classification scheme. Facilities in rural areas include those in micropolitan areas with an urban core of at least 10,000 but less than 50,000 population, as well as those in non-core areas. Facilities in a central or fringe urban core of 50,000 or more are considered urban. Facility operation was self-designated in N-SSATS Question 7. |
| FIGURE III.9. Percentage of Facilities Offering Opioid-Related and Any Pharmacotherapies, 2016 |
|---|
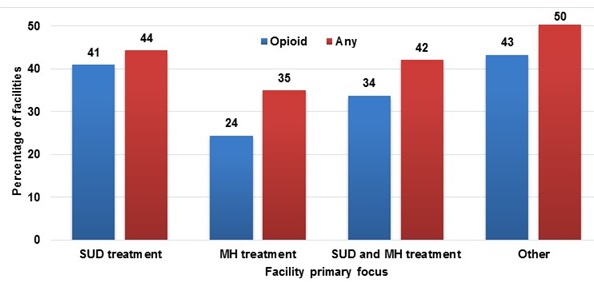 |
| SOURCE: N-SSATS 2016. NOTE: Facility focus was determined based on responses to Question 6. |
According to the SAMHSA-HRSA Center for Integrated Health Solutions (2014), several barriers limit the use of pharmacotherapy. These barriers include lack of available prescribers, agency regulatory policies that restrict or forbid pharmacotherapy use, provider workforce attitudes, insurer limits on dosages prescribed (that is, annual or lifetime medication limits), insurer authorization requirements, requirements that behavioral therapies be tried first, lack of support staff for providers administering pharmacotherapy, and inconsistent credentialing or licensure requirements for counseling staff to be reimbursed for pharmacotherapy-related services. Cunningham et al. (2009) identified somewhat different obstacles to widespread adoption of pharmacotherapy, including regulatory restrictions, lack of access to medical personnel trained in delivering such treatment, and physician reluctance. Friedman et al. (2012) identified lack of qualified medical staff as a reason for lack of pharmacotherapy in the criminal justice system. Roman et al. (2011) asserted that limited knowledge about SUD treatment medications among the public hinders its use. Mass media advertising of prescription medications for other health conditions has accelerated use of those medications; broader public knowledge of the benefits of pharmacotherapy for SUDs could encourage its more widespread use.
Mark et al. (2015) demonstrated how Medicaid coverage restrictions can be a substantial barrier to provision of pharmacotherapy. They analyzed data from 2013 Medicaid pharmacy documents, 2011 and 2012 Medicaid state drug utilization records, and a 2013 American Society of Addiction Medicine survey. Only 13 state Medicaid programs included all medications approved for alcohol and opioid dependence on their preferred drug lists. The most commonly excluded were extended-release naltrexone (19 programs), acamprosate (19 programs), and methadone (20 programs). Almost all Medicaid programs required prior authorization for combined buprenorphine-naloxone and had lifetime limits.
Many of the barriers to expansion of pharmacotherapy are related to the workforce. The number of medical staff qualified to provide pharmacotherapy services and the staff supporting them needs to increase for pharmacotherapy provision to expand. Training primary care providers to provide pharmacotherapy in primary care or other integrated care settings such as HIV or mental health clinics can improve treatment access and abstinence at six months (NIDA 2017; Korthuis et al. 2017). Primary care providers can act independently or work collaboratively with SUD treatment specialist in these models. In addition to increasing the number of qualified providers workforce attitudes toward pharmacotherapy, such as requiring behavioral therapies be tried first, need to change to attain widespread adoption. Last, consistent credentialing and licensure requirements are needed across states and insurers for professionals providing pharmacotherapy services. The HHS Opioid Strategy announced in April 2017 aims to continue the department's efforts to improve access to "treatment, and recovery services, including the full range of medication-assisted treatments" (HHS 2017); also, despite the barriers, the ACA has resulted in expansions in the number of physicians waivered to prescribe buprenorphine (Knudsen et al. 2015).
3. What is the Utilization Rate for Residential and Inpatient Beds Designated for SUD Treatment?
The N-SSATS reports the number of beds designated for SUD treatment in residential and inpatient hospital specialty treatment settings. Capacity in these care settings can be assessed by estimating a utilization rate based on the number of clients in care relative to the number of designated beds. Facilities providing outpatient care generally do not have a consistent definition of available capacity. Thus, we were not able to assess utilization rates in outpatient settings.
Despite increases in designated beds, treatment capacity in the residential and inpatient hospital settings appears insufficient to meet demand in 2015 (Table B.17). Nationally, there was a 4 percent increase in designated residential beds and a 26 percent increase in inpatient hospital beds between 2013 and 2015. Despite these increases, the utilization rate for residential beds increased from 97 percent to 106 percent and that for inpatient hospital beds from 97 percent to 109 percent.11 In 18 states, residential bed utilization rates across all facilities were over 100 percent in 2015; the same number of states had inpatient bed utilization rates over 100 percent.
C. What is the Current Capacity of SUD Treatment Organizations to Participate in Efforts to Integrate SUD Treatment within the Broader Health Care System? To What Degree are SUD Treatment Providers Used to Billing Medicaid?
Many SUD treatment providers have traditionally relied on grant funding. As potential clients obtain insurance coverage as a result of insurance coverage expansions, there is concern that providers are not prepared to accept Medicaid and private insurance. The N-SSATS annually asks specialty SUD treatment facilities what forms of payment they accept for services. The facilities represented in the N-SSATS are a census of public and private facilities with SUD treatment programs, including hospital, residential, and outpatient treatment providers. These facilities account for the majority of SUD treatment spending in the United States. Table III.2 identifies the percentage of these facilities that reported accepting private health insurance and Medicaid coverage in 2013 and 2016. Between 2013 and 2016, there was a small increase in the percentage of facilities accepting private health insurance (66 percent in 2013 versus 70 percent in 2016) and Medicaid insurance (60 percent in 2013 versus 63 percent in 2016). Small proportional increases in insurance acceptance occurred in all regions and across all facility types except "any inpatient setting." It is notable that there was no change in Medicaid acceptance in states that had less than a 10 percent increase in Medicaid enrollment or in "any inpatient setting."
| TABLE III.2. Percentage of Facilities Accepting Indicated Insurance Type | ||||||
|---|---|---|---|---|---|---|
| Facility Type | Proportion Accepting Private Health Insurance | Proportion Accepting Medicaid | ||||
| 2013 | 2016 | % Change | 2013 | 2016 | % Change | |
| Total | 66 | 70 | 4 | 60 | 63 | 5 |
| Urbanicity | ||||||
| Urban | 64 | 67 | 4 | 56 | 59 | 4 |
| Rural | 71 | 76 | 8 | 67 | 74 | 11 |
| Region | ||||||
| Northeast | 70 | 73 | 4 | 77 | 78 | 1 |
| Midwest | 76 | 78 | 2 | 64 | 67 | 5 |
| South | 61 | 63 | 4 | 56 | 58 | 3 |
| West | 60 | 64 | 8 | 47 | 51 | 9 |
| States in which Medicaid enrollment increased more than 10% between January 2014 and January 2015 | ||||||
| Yes | 63 | 66 | 5 | 53 | 59 | 10 |
| No | 69 | 71 | 4 | 65 | 65 | 0 |
| Operation | ||||||
| Private NP | 66 | 68 | 2 | 69 | 71 | 4 |
| Private FP | 64 | 69 | 8 | 41 | 45 | 10 |
| Public | 65 | 67 | 3 | 62 | 67 | 8 |
| Facility Setting | ||||||
| Outpatient only | 67 | 70 | 4 | 63 | 66 | 5 |
| Residential only | 46 | 50 | 9 | 40 | 41 | 4 |
| Residential and outpatient | 71 | 74 | 5 | 51 | 54 | 7 |
| Any inpatient hospital | 93 | 92 | -1 | 86 | 86 | 0 |
| SOURCE: N-SSATS, 2013 (Question 25) and 2016 (Question 27). NOTE: We calculated the percentage of facilities accepting private insurance and Medicaid by dividing the number of facilities reporting that they accept the indicated insurance type by the total number of facilities in the various categories. We excluded United States territories from the "Region" and "States in which Medicaid enrollment increased more than 10% between January 2014 and January 2015." We assigned urbanicity based on the National Center for Health Statistics urbanicity classification scheme. Facilities in rural areas include those in micropolitan areas with an urban core of at least 10,000 but less than 50,000 population, as well as those in non-core areas. Facilities in a central or fringe urban core of 50,000 or more are considered urban. Facility operation was self-designated in N-SSATS Question 4 in 2013 and Question 7 in 2016. |
||||||
D. How Have Wages for SUD Treatment Staff Changed Over the Last Decade?
Although most SUD counselors and social workers hold post-graduate degrees, average hourly wages for SUD treatment professionals are substantially lower than the average wage for all occupations. BLS collects hourly wage data in its Occupation Employment Survey (OES), including the following two occupational categories that include SUD counselors and social workers: (1) substance abuse and behavioral disorder counselors; and (2) mental health and substance abuse social workers. Wages for these two occupations have been below the average for all occupations for the last decade (Figure III.10). Trends in wage growth over the last decade resulted in expansion of these wage gaps for SUD treatment professionals, particularly substance abuse counselors:
-
2006 to 2009. Wages increased substantially for all occupations (3.5 percent annually) and for the occupations including SUD counselors (4.0 percent annually) and social workers (2.8 percent annually).
-
2009 to 2012. Wages of substance abuse counselors lost ground relative to other occupations, as there was little wage growth for the occupation category including them (0.4 percent annually). Wage growth continued for other occupations (1.7 percent annually), including substance abuse social workers (1.6 percent annually), albeit at a slower rate than in previous years. The lack of growth in this period was likely due to the economic recession and associated reductions in state revenue.
-
2012 and 2016. Slow wage growth continued for all occupations and those including SUD counselor and social worker occupation categories (about 1.8 percent annually). Wage growth for substance abuse counselors increased at the same rate as other occupations but did not make up for losses in wages relative to other occupations that occurred during the recession.
| FIGURE III.10. Trends in Wage Gaps for SUD Treatment Staff, BLS OES 2006-2016 |
|---|
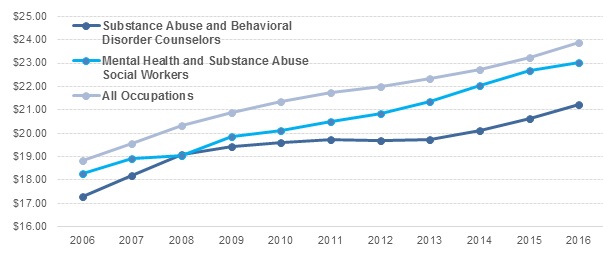 |
| SOURCE: BLS OES 2006-2016. NOTE: The OES is a semiannual survey measuring occupational employment and wage rates for wage and salary workers in non-farm establishments in the United States. The OES survey draws its sample from state unemployment insurance files. |
Over the last decade, these wage growth trends resulted in an expansion of the gap between the mean wage for all occupations and that for the occupation including SUD treatment counselors (from $1.56 to $2.63 per hour). The wage gap for social workers relative to other occupations has fluctuated over the years (from about $0.54 in 2015 to about $1.27 in 2008) (Figure III.11).
To provide specific example of wages for alternative career paths, we selected two health care professions requiring similar or fewer years of education. In 2016, the mean hourly wages for SUD counselors were $5 and $13 lower, respectively, than those for marriage and family therapists and registered nurses.
| FIGURE III.11. Gap Between Mean Hourly Wage for All Occupations and Occupations with SUD Treatment Staff, BLS OES 2006*2016 |
|---|
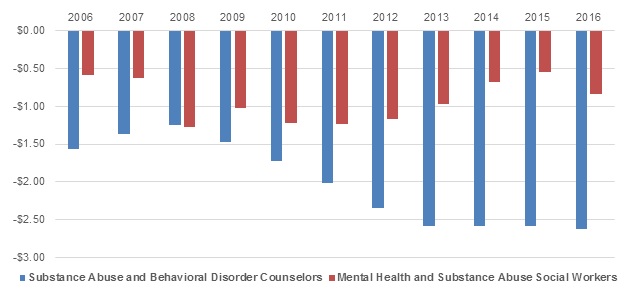 |
| SOURCE: BLS OES, 2006-2016. NOTE: The OES is a semiannual survey measuring occupational employment and wage rates for wage and salary workers in non-farm establishments in the United States. The OES survey draws its sample from state unemployment insurance files. |
The SUD treatment field's current high turnover rate is commonly attributed to inadequate compensation. Compensation for behavioral health professionals is significantly lower than for other health and non-health professions requiring similar levels of training (Hyde 2013; Bukach 2017). The clinical directors interviewed as part of the national Vital Signs survey of specialty SUD treatment facilities noted that low compensation makes hiring and retaining qualified staff a challenge (Ryan et al. 2012). Efforts to increase the labor supply in the SUD treatment field through training programs without an associated increase in reimbursement for services through insurance or other funding sources are likely to result in reduced wage levels and even lower retention as individuals in the SUD treatment field recognize the potential to increase their earnings by shifting to other professions.
IV. DISCUSSION
Policymakers at all levels of government have targeted increasing SUD treatment use to address escalating drug overdose deaths related to the opioid epidemic and improve societal welfare. Meanwhile, rates of SUD treatment use generally have been constant for more than a decade despite the substantial recent increase in insurance coverage for SUD treatment. Individuals with SUD treatment needs overwhelmingly indicate that they do not feel a need for treatment and, even among the small minority who believe that they might benefit from treatment, most make no effort to obtain it. Thus, expanding treatment use will require a multifaceted approach including increasing public awareness of treatment effectiveness, reducing stigma associated with SUD treatment, addressing financial barriers, and increasing primary care physicians' role in screening, treatment and referral.
On the supply side, low wage rates for SUD treatment professionals are associated with high turnover and difficulty in hiring qualified staff. Individuals trained to provide SUD treatment quickly move on to other professions that offer better working conditions, wages, and benefits (Hyde 2013; Ryan et al. 2012; Bukach 2017). There is also concern that low treatment reimbursement rates and restrictions on SUD treatment coverage under Medicaid may be a barrier to expanding treatment in some states (Dickson 2015).
Overall, the role of Medicaid in funding SUD treatment services has expanded since 2014 although many of the individuals who gained Medicaid coverage would have received SUD treatment through another funding source such as state and local funding or federal block grants. In parallel to this shift in funding source there has been a shift from care provision in publicly operated facilities to increased use of privately operated facilities. There is an opportunity for policymakers to redirect the public funding and resources to activities encouraging expanded treatment use and providing a continuum of care that addresses the chronic nature of SUDs. Likewise state Medicaid programs have the potential to play an important role in transforming the SUD treatment system and HHS Centers for Medicare and Medicaid Services (CMS) is taking an active role encouraging states to make reforms. CMS is conducting an Innovation Accelerator Program (IAP) to support state efforts to expand SUD treatment under Medicaid. The IAP supports efforts to improve care quality and continuity, enhance performance monitoring capacity, identify beneficiaries in need of treatment, develop a continuum of care that addresses the variety treatment needs and the chronic nature of SUDs, and target reimbursement models to incentivize better outcomes (CMS 2017). In addition, CMS has been working with states to improve access to and quality of SUD treatment through Medicaid Section 1115 demonstrations (CMS 2017b).
The impact of a number of recent federal efforts to increase SUD treatment use and the quality of SUD treatment services is not fully captured in the data available for this study. The initiatives include the CMS IAP program as well as several SAMHSA grant programs intended to expand access to SUD treatment (McCance-Katz et al. 2017). The Opioid State Targeted Response grants provided $485 million to states and United States territories in fiscal year 2017 primarily to expand treatment, recovery support and prevention activities. The Medication-Assisted Treatment for Prescription Drug and Opioid Addiction program expands pharmacotherapy access by providing grants to states with the highest rates of treatment admissions for opioid addiction. There are also a number of federally-funded efforts to expand access to SUD screening and treatment in primary care settings and rural areas including integrating SUD treatment into community mental health centers, use of telemedicine, efforts to educate primary care providers on addiction risks and treatment, partnerships between primary care and specialty providers, and expansion of buprenorphine waivered primary care providers and the number of patients that can be treated under each waiver. Future years of data should be monitored to assess the impact of these initiatives.
REFERENCES
Barnett, J.C., and E.R. Berchick. "Health Insurance Coverage in the United States." Current Population Reports, P60-260. Washington, DC: U.S. Government Publishing Office, 2017.
Baser, O., M. Chalk, D.A. Fiellin, and D.R. Gastfriend. "Cost and Utilization Outcomes of Opioid-Dependence Treatments." American Journal of Managed Care, vol. 17, Suppl 8, 2011, pp. S235-48.
Batts, K., M. Pemberton, J. Bose, B. Weimer, L. Henderson, M. Penne, J. Gfroerer, D. Trunzo, and A. Strashny. "Comparing and Evaluating Substance Use Treatment Utilization Estimates from the National Survey on Drug Use and Health and Other Data Sources." Rockville, MD: Substance Abuse and Mental Health Services Administration, 2014.
Beronio, K., S. Glied, and R. Frank. "How the Affordable Care Act and Mental Health Parity and Addiction Equity Act Greatly Expand Coverage of Behavioral Health Care." Journal of Behavioral Health Services and Research, vol. 41, no. 4, 2014, pp. 410-428.
Bouchery, E.E., R. Morris, and J. Little. "Examining Substance Use Disorder Treatment Demand and Provider Capacity in a Changing Health Care System: Initial Findings Report." Report prepared for the HHS Office of the Assistant Secretary for Planning and Evaluation. Washington, DC: Mathematica Policy Research, September 30, 2015. Available at https://aspe.hhs.gov/report/examining-substance-use-disorder-treatment-demand-and-provider-capacity-changing-health-care-system-initial-findings-report.
Bouchery, E.E., H.J. Harwood, J. Dilonardo, and R. Vandivort-Warren. "Type of Health Insurance and the Substance Abuse Treatment Gap." Journal of Substance Abuse Treatment, vol. 42, no. 3, 2012, pp. 289-300.
Brubaker, M.D., E.A. Amatea, E. Torres Rivera, M.D. Miller, and L. Nabors. "Barriers and Supports to Substance Abuse Service Use Among Homeless Adults." Journal of Addictions and Offender Counseling, vol. 34, no. 2, 2013, pp. 81-98.
Brugal, M.T., A. Domingo-Salvany, R. Puig, G. Barrio, P. Garcia de Olalla, and L. de la Fuente. "Evaluating the Impact of Methadone Maintenance Programmes on Mortality Due to Overdose and AIDS in a Cohort of Heroin Users in Spain. Addiction, vol. 100, no. 7, 2005, pp. 981-989. doi: 10.1111/j.1360-0443.2005.01089.x.
Bukach, A.M., F.K. Ejaz, N. Dawson, and R.J. Gitter. "Turnover among Community Mental Health Workers in Ohio." Administration and Policy in Mental Health, vol. 44, 2017, pp. 115-122. doi: 10.1007/s10488-015-0706-1.
Center for Behavioral Health Statistics and Quality. "2013-2014 National Surveys on Drug Use and Health: Model-Based Estimated Totals (in Thousands)." Rockville, MD: Substance Abuse and Mental Health Services Administration, 2015.
Center for Behavioral Health Statistics and Quality. "2014 National Survey on Drug Use and Health: Detailed Tables." Rockville, MD: Substance Abuse and Mental Health Services Administration, 2015a.
Center for Behavioral Health Statistics and Quality. "2015 National Survey on Drug Use and Health: Detailed Tables." Rockville, MD: Substance Abuse and Mental Health Services Administration, 2016.
Center for Behavioral Health Statistics and Quality. "Key Substance Use and Mental Health Indicators in the United States: Results from the 2015 National Survey on Drug Use and Health." Rockville, MD: Substance Abuse and Mental Health Services Administration, 2016b.
Center for Behavioral Health Statistics and Quality. "Treatment Episode Data Set Discharges (TEDS-D), 2012: Codebook." Available at https://wwwdasis.samhsa.gov/dasis2/teds_pubs/TEDS/Discharges/TED_D_2012/teds_d_2012_codebook.pdf. Accessed on November 22, 2017a.
Center for Behavioral Health Statistics and Quality. "Treatment Episode Data Set Discharges (TEDS-D), 2014: Codebook." Available at https://wwwdasis.samhsa.gov/dasis2/teds_pubs/TEDS/Discharges/TED_D_2014/teds_d_2014_codebook.pdf. Accessed on November 22, 2017b.
Centers for Medicare and Medicaid Services. "Medicaid Innovation Accelerator Program: Reducing Substance Use Disorders." Available at https://www.medicaid.gov/state-resource-center/innovation-accelerator-program/iap-downloads/learn-hilc-iap.pdf. Accessed on November 14, 2017.
Centers for Medicare and Medicaid Services. "Strategies to Address the Opioid Epidemic. SMD #17-003" Available at https://www.medicaid.gov/federal-policy-guidance/downloads/smd17003.pdf. Accessed on November 14, 2017.
Clark, R.E., M. Samnaliev, J.D. Baxter, and G.Y. Leung. "The Evidence Doesn't Justify Steps by State Medicaid Programs to Restrict Opioid Addiction Treatment with Buprenorphine." Health Affairs, vol. 30, no. 8, 2011, pp. 1425-1433. doi: 10.1377/hlthaff.2010.0532.
Cousins, G., F. Boland, B. Courtney, J. Barry, S. Lyons, and T. Fahey. "Risk of Mortality On and Off Methadone Substitution Treatment in Primary Care: A National Cohort Study." Addiction, vol. 111, no. 1, 2016, pp. 73-82. doi: 10.1111/add.13087.
Cummings, J.R., H. Wen, M. Ko, and B.G. Druss. "Race/Ethnicity and Geographic Access to Medicaid Substance Use Disorder Treatment Facilities in the United States." JAMA Psychiatry, vol. 71, no. 2, 2014, pp. 190-196.
Cunningham, C.O., A. Giovanniello, G. Sacajui, X. Li, M. Brisbane, and N.L. Sohler. "Inquiries About and Initiation of Buprenorphine Treatment in an Inner-City Clinic." Substance Abuse, vol. 30, no. 3, 2009, pp. 261-262.
Degenhardt, L., D. Randall, W. Hall, M. Law, T. Butler, and L. Burns. "Mortality Among Clients of a State-Wide Opioid Pharmacotherapy Program over 20 Years: Risk Factors and Lives Saved." Drug and Alcohol Dependence, vol. 105, nos. 1-2, 2009, pp. 9-15. doi: 10.1016/j.drugalcdep.2009.05.021.
Dickson, V. "Medicaid Plans Struggle to Provide Mental Health Services." Modern Healthcare. Available at http://www.modernhealthcare.com/article/20150704/MAGAZINE/307049979. Accessed on November 15, 2017.
Dilonardo, J. "Workforce Issues in Integrated Behavioral Healthcare: A Background Paper." National Council for Community Behavioral Healthcare, 2011 unpublished paper.
"DSM-IV-TR Criteria for Substance Abuse and Substance Dependence." Clinical Tools, Inc. Available at https://www.buppractice.com/node/1436. Accessed on November 15, 2017.
Elinson, Z. "Aging Baby Boomers Bring Drug Habits Into Middle Age." Wall Street Journal, March 16, 2015.
Fiellin, D.A., R.S. Schottenfeld, C.J. Cutter, B.A. Moore, D.T. Barry, and P.G. O'Connor. "Primary Care-Based Buprenorphine Taper vs. Maintenance Therapy for Prescription Opioid Dependence: A Randomized Clinical Trial." JAMA Internal Medicine, vol. 174, no. 12, 2014, pp. 1947-1954. doi: 10.1001/jamainternmed.2014.5302.
Foster, S.E. "Institute of Medicine-National Resource Council Workshop on Improving the Health, Safety and Well-Being of Young Adults." January 2014. Available at https://iom.nationalacademies.org/~/media/Files/Activity%20Files/Children/ImprovingYoungAdultsHealth/Foster%20Presentation.pdf. Accessed August 16, 2015.
Friedman, P.D., R. Hoskinson Jr., M. Gordon, R. Schwartz, T. Kinlock, K. Knight, P.M. Flynn, W.N. Welsh, L.A.R. Stein, S. Sacks, D.J. O'Connell, H.K. Knudsen, M.S. Shafer, E. Hall, and L.K. Frisman. "Medication-Assisted Treatment in Criminal Justice Agencies Affiliated with the Criminal Justice-Drug Abuse Treatment Studies (CJ-DATS): Availability, Barriers, and Intentions." Substance Abuse, vol. 33, no. 1, 2012, pp. 9-18.
Han, B.H., A.A. Moore, S. Sherman, K.M. Keyes, ans J.J. Palamar. "Demographic Trends of Binge Alcohol Use and Alcohol Use Disorders among Older Adults in the United States, 2005-2014." Drug and Alcohol Dependence, vol. 170, pp. 198-207.
Humphreys, K., and R.G. Frank. "The Affordable Care Act Will Revolutionize Care for Substance Use Disorders in the United States." Addiction, vol. 109, no. 12, 2014, pp. 1957-1958.
Hyde, P.S. "Report to Congress on the Nation's Substance Abuse and Mental Health Workforce Issues." Rockville, MD: Substance Abuse and Mental Health Services Administration, January 24, 2013.
Institute of Medicine. "Improving the Quality of Health Care for Mental and Substance-Use Conditions." Washington, DC: National Academies Press, 2006.
Jackson, A., and L. Shannon. "Examining Barriers to and Motivations for Substance Abuse Treatment Among Pregnant Women: Does Urban-Rural Residence Matter?" Women and Health, vol. 52, no. 6, 2012, pp. 570-586.
Knudsen, H.K., M.R. Lofwall, J.R. Havens, and S.L. Walsh. "States' Implementation of the Affordable Care Act and the Supply of Physicians Waivered to Prescribe Buprenorphine for Opioid Dependence." Drug and Alcohol Dependence, vol. 157, 2015, pp. 36-43.
Korthuis, P.T., D. McCarty, M. Weimer, C. Bougatsos, I. Blazina, B. Zakher, et al. Primary Care-Based Models for the Treatment of Opioid Use Disorder: A Scoping Review. Ann Intern Med, 2017, vol. 166, pp. 268-278. doi: 10.7326/M16-2149
Larson, M.J., A. Zhang, K. Smith, and L. Kasten. "Access to Services: Multiple Perspectives from Adults with Substance Abuse Disorders in Massachusetts." Administration and Policy in Mental Health, vol. 32, no. 4, 2005, pp. 357-371.
Lenardson, J.D., and J.A. Gale. "Distribution of Substance Abuse Treatment Facilities Across the Rural-Urban Continuum." Maine Rural Health Research Center, Working paper #35, Institute for Health Policy, Muskie School of Public Service, University of Southern Maine, 2007.
Lewin Group and National Opinion Research Center. "Survey of Substance Abuse Treatment Providers as Information Consumers." Report prepared for Substance Abuse and Mental Health Services Administration, 2000.
Lipari, R.N., E. Park-Lee, and S. Van Horn. "America's Need for and Receipt of Substance Use Treatment in 2015." Rockville, MD: Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality, September 29, 2016.
MacMaster, S.A. "Perceptions of Need, Service Use, and Barriers to Service Access among Female Methamphetamine Users in Rural Appalachia." Social Work in Public Health, vol. 28, no. 2, 2013, pp. 109-118.
Mann, C., T. Frieden, P.S. Hyde, N.D. Volkow, and G.F. Koob. "Subject: Medication Assisted Treatment for Substance Use Disorders." 2014. Available at http://www.medicaid.gov/Federal-Policy-Guidance/Downloads/CIB-07-11-2014.pdf. Accessed August 16, 2015.
Mark, T.L., R. Lubran, E.F. McCance-Katz, M. Chalk, and J. Richardson. "Medicaid Coverage of Medications to Treat Alcohol and Opioid Dependence." Journal of Substance Abuse Treatment, vol. 55, 2015, pp. 1-5.
McCarty, D. "The Alcohol and Drug Abuse Treatment Workforce." Frontlines: Linking Alcohol Services Research and Practice, vol. 5, no. 8, 2002, p. 2.
McCance-Katz, Elinore, Deborah Houry, Francis Collins, and Scott Gottlieb. "Testimony on the Federal Response to the Opioid Crisis before Committee on Health, Education, Labor and Pensions." Available at http://www.hhs.gov/about/agencies/asl/testimony/2017-10/federal-respons…. Accessed on November 14, 2017.
Mechanic, D. "Is the Prevalence of Mental Disorders a Good Measure of the Need for Services?" Health Affairs, vol. 22, no. 5, 2003, pp. 8-20.
Mojtabai, R. "Use of Specialty Substance Abuse and Mental Health Services in Adults with Substance Use Disorders in the Community." Drug and Alcohol Dependence, vol. 78, no. 3, 2005, pp. 345-354.
National Association of State Alcohol and Drug Abuse Directors. "State Regulations on Substance Use Disorder Programs and Counselors: An Overview." Washington, DC: National Association of State Alcohol and Drug Abuse Directors, 2013.
Newhouse, J.P., and the Insurance Experiment Group. "Free for All? Lessons from the RAND Health Experiment." Cambridge, MA: Harvard University Press, 1993.
National Institute on Drug Abuse. "Collaborative Care Shows Promise for Opioid and Alcohol Use Disorders." Available at https://www.drugabuse.gov/news-events/news-releases/2017/08/collaborative-care-shows-promise-opioid-alcohol-use-disorders. Access November 17, 2017.
Peterson, J.A., R.P. Schwartz, S.G. Mitchell, H.S. Reisinger, S.M. Kelly, K.E. O'Grady, B.S. Brown, and M.H. Agar. "Why Don't Out-of-Treatment Individuals Enter Methadone Treatment Programmes?" International Journal of Drug Policy, vol. 21, no. 1, 2010, pp. 36-42.
Pierce, M., S.M. Bird, M. Hickman, J. Marsden, G. Dunn, A. Jones, and T. Millar. "Impact of Treatment for Opioid Dependence on Fatal Drug-Related Poisoning: A National Cohort Study in England." Addiction, vol. 111, no. 2, 2016, pp. 298-308. doi: 10.1111/add.13193.
Roman, P.M., A.J. Abraham, and H.K. Knudsen. "Using Medication-Assisted Treatment for Substance Use Disorders: Evidence of Barriers and Facilitators of Implementation." Addiction Behavior, vol. 36, no. 6, 2011, pp. 584-589.
Rudd, R.A., N. Aleshire, J.E. Zibbell, and R.M. Gladden. "Increases in Drug and Opioid Overdose Deaths--United States, 2000-2014." Morbidity and Mortality Weekly Report, vol. 64, no. 50, January 1, 2016, pp. 1378-1382. Available at https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6450a3.htm. Accessed October 16, 2017.
Ryan, O., D. Murphy, and L. Krom. "Vital Signs: Taking the Pulse of the Addiction Treatment Workforce, A National Report," Version 1. Kansas City, MO: Addiction Technology Transfer Center National Office, University of Missouri-Kansas City, 2012.
SAMHSA-HRSA Center for Integrated Health Solutions. "Expanding the Use of Medications to Treat Individuals with Substance Use Disorders in Safety-Net Settings Creating Change on the Ground: Opportunities and Lessons Learned from the Field." 2014.
Saum, C.A., M.L. Hiller, M.E. Leigey, J.A. Inciardi, and H.L. Surratt. "Predictors of Substance Abuse Treatment Entry for Crime-Involved, Cocaine-Dependent Women." Drug and Alcohol Dependence, vol. 91, no. 2, 2007, pp. 253-259.
Schmidt, L.A., and C.M. Weisner. "Private Insurance and the Utilization of Chemical Dependency Treatment." Journal of Substance Abuse Treatment, vol. 28, no. 1, 2005, pp. 67-76.
Stevens, J.P., M.J. Wall, L. Novack, J. Marshall, D.J. Hsu, and M.D. Howell. "The Critical Care Crisis of Opioid Overdoses in the United States." American Thoracic Society. Available at http://www.thoracic.org/about/newsroom/press-releases/resources/opioid-crisis-and-icus.pdf. Accessed October 16, 2017.
Substance Abuse and Mental Health Services Administration. "Alcohol and Drug Services Study (ADSS): The National Substance Abuse Treatment System: Facilities, Clients, Services, and Staffing." Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies, 2003.
Substance Abuse and Mental Health Services Administration. "Treatment Episode Data Set (TEDS): 2004-2014. State Admissions to Substance Abuse Treatment Services." BHSIS Series S-85, HHS Publication No. (SMA) 16-4987. Rockville, MD: Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality, 2016.
U.S. Department of Agriculture. "Rural America at a Glance." Economic Information Bulletin: U.S. Department of Agriculture, Economic Research Service, 162, 2016. Available at https://www.ers.usda.gov/webdocs/publications/80894/eib-162.pdf?v=42684. Accessed October 16, 2017.
Wu, L.T., and C. Ringwalt. "Use of Substance Abuse Services by Young Uninsured American Adults." Psychiatry Online, vol. 56, no. 8, 2005, pp. 946-953.
Xu, J., R.C. Rapp, J. Wand, and R.G. Carlson. "The Multidimensional Structure of External Barriers to Substance Abuse Treatment and its Invariance Across Gender, Ethnicity, and Age." Substance Abuse, vol. 29, no. 1, 2008, pp. 43-54. doi: 10.1300/J465v29n07_06.
NOTES
-
SAMHSA did not count positive responses to NSDUH questions regarding treatment at an emergency room, private doctor's office, self-help group, prison or jail, or hospital as an outpatient as specialty treatment.
-
For the NSDUH SAMHSA defines specialty treatment based on the setting of care as described above. The N-SSATS universe is limited to specialty treatment facilities. These facilities have units or programs focused on provision of SUD treatment. Thus, facilities may not be defined as "specialty" in both surveys. For example, a general hospital or mental health center would not be included in the N-SSATS universe unless they have a treatment program or unit designated for SUD treatment. These settings are, however, consider specialty treatment for NSDUH.
-
Stevens et al. (2017) found a 34 percent increase in opioid overdose-related admissions to hospital intensive care units between January 2009 and September 2015 in a study of 162 hospitals in 44 states.
-
We define an FTE as 40 working hours per week.
-
N-SSATS surveys the universe of specialty SUD treatment facilities. In 2016 the survey had a 91 percent response rate. Estimates are not adjusted for facility or item non-response.
-
Utilization rate is calculated by dividing the number of clients in care by the total number of designated beds. The utilization rate will exceed 100 percent when clients are placed in beds not specifically designated for substance use treatment.
-
The survey instrument is available at https://wwwdasis.samhsa.gov/dasis2/nssats/nssats_2016_q.pdf.
-
SAMHSA did not include emergency room, private doctor's office, self-help group, prison or jail, or hospital as an outpatient in the definition of specialty settings.
-
For the NSDUH SAMHSA defines specialty treatment based on the setting of care as listed above. The N-SSATS universe is limited to specialty treatment facilities. These facilities have units or programs focused on provision of SUD treatment. Thus, facilities may not be defined as "specialty" in both surveys. For example, a general hospital or mental health center would not be included in the N-SSATS universe unless they have a treatment program or unit designated for SUD treatment. These settings are, however, consider specialty treatment for NSDUH.
-
We conducted a logistic regression using data from the 2009-2014 NSDUH to estimate the increase in the likelihood of receiving treatment that was associated with being enrolled in Medicaid relative to being uninsured. The regression controlled for age, gender, race/ethnicity, education level, household income, marital status, age of first alcohol/illicit drug use, cigarette use, criminal activity, health status, population density, work status, SUD type, and year. Holding all other characteristics constant at the average for the population, the regression analysis indicated that, at the margin, the likelihood of specialty SUD treatment for someone who was uninsured was 60 percent of that for an individual who was Medicaid insured.
-
Utilization rate is calculated by dividing the number of clients in care by the total number of designated beds. The utilization rate will exceed 100 percent when clients are placed in beds not specifically designated for substance use treatment.
APPENDIX A: DATA SOURCES
In this appendix, we provide a brief description of the three data sources we used to develop the analyses in this report.
A. National Survey of Substance Abuse Treatment Services (N-SSATS)
The N-SSATS is an ideal source for analyzing trends in clients who are receiving specialty SUD treatment as well as trends in SUD treatment facility characteristics. It is an annual survey of the universe of specialty SUD treatment facilities. Counts of clients in care (on the last working day in March of each survey year) were collected annually through 2013 and biannually thereafter. Key strengths of the survey include its comprehensiveness in terms of the inclusion of facilities and the types of information collected. The N-SSATS, which includes all known specialty SUD treatment facilities in the United States, consistently achieves response rates greater than 90 percent. This allows for detailed analysis of small states or subgroups.
The N-SSATS data, however, are limited in several ways. Specifically, N-SSATS excludes non-specialty providers, solo practitioners, and facilities serving only criminal justice populations. The exclusion of solo practitioners might be particularly important to analysis of programs such as those implementing Hub and Spoke models, which seek to increase treatment access at non-specialty providers. The exclusion of facilities that target only criminal justice populations might limit the potential for analyzing programs that target people exiting criminal justice institutions; however, many of these people might be served by facilities included in N-SSATS. N-SSATS does include information on whether facilities have programs that focus on criminal justice clients (excluding programs for those convicted of driving under the influence/driving while intoxicated).
The N-SSATS estimates presented in this report were directly extracted from N-SSATS reports and special tabulations. We summarize the data presented in those reports or present tabulations produced by the SAMHSA from the workforce questions and other questions included in the N-SSATS 2016 survey. For example, Mathematica assigned states to a category identifying "States in which Medicaid enrollment increased more than 10 percent between January 2014 and January 2015" or not based on Medicaid enrollment reports. Then client counts from the N-SSATS reports were summarized for the states in each group to produce the estimates for these categories reported in Appendix B.
B. National Survey on Drug Use and Health (NSDUH)
The NSDUH is designed to track the prevalence of SUDs in the United States by type of substance. The NSDUH is an annual survey of the civilian, non-institutionalized population ages 12 and older in the United States. As a population survey, it provides the most comprehensive information about the number of people who meet diagnostic criteria for an SUD, who misuse prescription opioids, and who have accessed any SUD treatment service in the past year. The NSDUH includes a sufficient sample of respondents to develop state-level estimates when two years of survey data are combined; however, standard errors for estimates are often quite large for smaller states, making it impossible to identify small changes in disorder prevalence or treatment use.
There are a number of limitations to the NSDUH survey data. NSDUH provides limited information on the type of substance use treatment services received and no information on the intensity of services that respondents received. The survey excludes people who are homeless and not in a shelter, as well as those who are institutionalized, including those residing in hospitals, residential treatment settings, jails, or prisons. NSDUH does include individuals who have been released from prison or institutional care. Overall, estimates of the prevalence of alcohol and illicit drug use disorders based on the NSDUH reflect the household population only, and thus, are likely to understate national prevalence since groups with high prevalence are excluded. In addition to the exclusion of the subpopulations that have higher prevalence of SUDs (Office of Applied Studies 2002), the self-reported nature of the data collection likely results in some underreporting (Harrell 1997).
SAMHSA redesigned the NSDUH between the 2014 and 2015 surveys. Due to methodological changes associated with the redesign estimates from 2015 and later years are not comparable to earlier years. Updates to the prescription drug questions were a key component of the redesign (Center for Behavioral Health Statistics and Quality 2015):
-
Beginning in 2015, prescription drug questions were restructured to collect more information on use and misuse of specific prescription drugs. The definition of misuse was also changed with respondents being given more specific examples of misuse. In particular, prior to 2015 the definition of misuse did not include overuse of prescribed medication.
-
Methamphetamine was included as a prescription stimulant prior to 2015. However, most methamphetamine that is used in the United States is manufactured illegally, not prescribed. Therefore, beginning in 2015, a new methamphetamine module was added to address both prescription and non-prescribed use.
-
To help respondents categorize substances, the term "Molly" was added to questions about Ecstasy use in the hallucinogens module and use of felt tip pens and computer keyboard cleaner were added to the inhalants module.
The redesign also affected the abuse and dependence modules in the following key ways:
-
The logic for routing individuals to the substance abuse and dependence modules was updated.
-
Sedative withdrawal was updated to require two or more symptoms of withdrawal instead of one or more.
-
Dependence and abuse questions were added for methamphetamine.
The NSDUH estimates presented in this report were directly extracted from NSDUH reports prepared by SAMHSA or summarize data presented in those reports, with the exception of the analysis of Medicaid coverage in Section II.D.
C. Treatment Episode Data Set (TEDS)
Relative to the N-SSATS and the NSDUH, the TEDS provides more detailed information on treatment services and the characteristics of clients at admission and discharge. The TEDS aggregates admissions data collected in individual state administrative data systems. States collect these data to monitor their SUD treatment systems. Reporting requirements can vary substantially by state. Generally, facilities that receive public funds or that are licensed or certified by a state substance abuse agency are included in the state administrative systems. The universe of their admissions is reported to TEDS. The scope of facilities reporting in a given state may change over time.
REFERENCES
Center for Behavioral Health Statistics and Quality. "National Survey on Drug Use and Health: 2014 and 2015 Redesign Changes." Rockville, MD: Substance Abuse and Mental Health Services Administration, 2015.
Harrell, A.V. "The Validity of Self-Reported Drug Use Data: The Accuracy of Responses on Confidential Self-Administered Answer Sheets." In The Validity of Self-Reported Drug Use: Improving the Accuracy of Survey Estimates, edited by L. Harrison and A. Hughes. NIH Publication No. 97-4147, NIDA Research Monograph 167. Rockville, MD: National Institute on Drug Abuse, 1997, pp. 37-58.
Office of Applied Studies. "Results from the 2001 National Household Survey on Drug Abuse: Volume I; Summary of National Findings." NHSDA Series H-17, DHHS Publication No. SMA. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2002.
APPENDIX B: DETAILED TABLES
| TABLE B.1. Distribution of Specialty Treatment Receipt by Geographic Location and Type of Service, 2013 and 2015 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Geographic Area | Total | Outpatient | Residential | Inpatient | ||||||||
| 2013 | 2015 | % Change | 2013 | 2015 | % Change | 2013 | 2015 | % Change | 2013 | 2015 | % Change | |
| Total | 1,249,629 | 1,305,647 | 4.5 | 1,127,235 | 1,161,456 | 3.0 | 107,727 | 119,900 | 11.3 | 14,667 | 24,291 | 65.6 |
| States in which Medicaid enrollment increased more than 10% between January 2014 and January 2015 | ||||||||||||
| Yes | 595,725 | 632,949 | 6.2 | 541,402 | 570,134 | 5.3 | 48,288 | 51,953 | 7.6 | 6,035 | 10,862 | 80.0 |
| No | 638,421 | 661,025 | 3.5 | 573,454 | 583,257 | 1.7 | 56,877 | 64,933 | 14.2 | 8,090 | 12,835 | 58.7 |
| Region | ||||||||||||
| Northeast | 320,089 | 333,922 | 4.3 | 290,975 | 298,862 | 2.7 | 24,956 | 26,535 | 6.3 | 4,158 | 8,525 | 105.0 |
| Midwest | 257,983 | 262,161 | 1.6 | 234,244 | 240,128 | 2.5 | 21,603 | 19,539 | -9.6 | 2,136 | 2,494 | 16.8 |
| South | 345,446 | 377,894 | 9.4 | 308,139 | 328,054 | 6.5 | 31,593 | 40,582 | 28.5 | 5,714 | 9,258 | 62.0 |
| West | 310,628 | 319,997 | 3.0 | 281,498 | 286,347 | 1.7 | 27,013 | 30,230 | 11.9 | 2,117 | 3,420 | 61.5 |
| Urbanicity | ||||||||||||
| Urban | 954,890 | 1,103,406 | 15.6 | 860,436 | 979,226 | 13.8 | 83,150 | 102,633 | 23.4 | 11,304 | 21,547 | 90.6 |
| Rural | 279,167 | 190,478 | -31.8 | 254,331 | 174,075 | -31.6 | 22,015 | 14,253 | -35.3 | 2,821 | 2,150 | -23.8 |
| Operation | ||||||||||||
| Private, NP | 638,858 | 670,593 | 5.0 | 553,157 | 570,450 | 3.1 | 79,714 | 88,260 | 10.7 | 5,987 | 11,883 | 98.5 |
| Private, FP | 430,362 | 475,531 | 10.5 | 407,562 | 447,302 | 9.8 | 17,292 | 21,375 | 23.6 | 5,508 | 6,854 | 24.4 |
| Public | 180,409 | 159,523 | -11.6 | 166,516 | 143,704 | -13.7 | 10,721 | 10,265 | -4.3 | 3,172 | 5,554 | 75.1 |
| SOURCE: N-SSATS 2013 and 2015. NOTE: Inpatient and residential client counts represent the number of clients receiving services on March 31 of the indicated year (see Questions 28a and 29a in N-SSATS 2013 and Questions 29a and 30a in N-SSATS 2015). Outpatient client counts represent the number of clients who received outpatient services in March of the indicated year and who were still enrolled in care at the facility where they received those services on March 31 (see Question 30a in N-SSATS 2013 and Question 31a in N-SSATS 2015). Total clients is the sum of inpatient, residential, and outpatient clients. United States territories are excluded from the categories for: (1) region; and (2) states in which Medicaid enrollment increased more than 10% between January 2014 and January 2015. The percent increase in Medicaid enrollment for each state was determined based on Medicaid enrollment reports. Therefore, the totals for these categories are lower than the reported total in the first line of the table. Urbanicity is assigned based on the National Center for Health Statistics urbanicity classification scheme. Facilities in rural areas include those in micropolitan areas with an urban core population of at least 10,000 but less than 50,000, as well as those in non-core areas. Facilities in a central or fringe urban core with a population of 50,000 or more are considered urban. Information on urbanicity was not available for all facilities; urban and rural client counts are only reported for facilities with known urbanicity. Facility operation was self-designated in N-SSATS Question 4 in 2013 and Question 7 in 2015. |
||||||||||||
| TABLE B.2. Distribution of Specialty Treatment Receipt by State and Type of Service, 2013 and 2015 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| State | % Change in Medicaid Enrollment (Jan 2014 to Jan 2015)a |
Total | Outpatient | Residential | Inpatient | ||||||||
| 2013 | 2015 | % Change | 2013 | 2015 | % Change | 2013 | 2015 | % Change | 2013 | 2015 | % Change | ||
| Total | 14.1 | 1,249,629 | 1,305,647 | 4.5 | 1,127,235 | 1,161,456 | 3.0 | 107,727 | 119,900 | 11.3 | 14,667 | 24,291 | 65.6 |
| Alabama | 8.9 | 15,089 | 14,548 | -3.6 | 13,632 | 13,125 | -3.7 | 1,205 | 1,391 | 15.4 | 252 | 32 | -87.3 |
| Alaska | 7.0 | 3,900 | 3,363 | -13.8 | 3,531 | 2,932 | -17.0 | 359 | 431 | 20.1 | 10 | NA | NA |
| Arizona | 22.8 | 31,832 | 33,978 | 6.7 | 29,449 | 30,671 | 4.1 | 2,016 | 2,845 | 41.1 | 367 | 462 | 25.9 |
| Arkansas | 9.7 | 5,927 | 7,154 | 20.7 | 5,124 | 4,704 | -8.2 | 715 | 2,415 | 237.8 | 88 | 35 | -60.2 |
| California | 24.0 | 117,159 | 111,961 | -4.4 | 101,899 | 95,834 | -6.0 | 14,300 | 14,156 | -1.0 | 960 | 1,971 | 105.3 |
| Colorado | 26.5 | 42,256 | 34,793 | -17.7 | 40,306 | 33,452 | -17.0 | 1,804 | 1,186 | -34.3 | 146 | 155 | 6.2 |
| Connecticut | 4.1 | 33,267 | 37,817 | 13.7 | 31,148 | 35,970 | 15.5 | 1,823 | 1,540 | -15.5 | 296 | 307 | 3.7 |
| Delaware | 3.4 | 5,278 | 10,327 | 95.7 | 4,969 | 6,495 | 30.7 | 170 | 3,800 | 2135.3 | 139 | 32 | -77.0 |
| District of Columbia | 9.1 | 3,833 | 2,824 | -26.3 | 3,324 | 2,392 | -28.0 | 468 | 431 | -7.9 | 41 | 1 | -97.6 |
| Florida | 9.1 | 53,641 | 63,287 | 18.0 | 45,069 | 51,823 | 15.0 | 7,786 | 8,531 | 9.6 | 786 | 2,933 | 273.2 |
| Georgia | 1.3 | 24,003 | 25,379 | 5.7 | 21,630 | 22,845 | 5.6 | 2,062 | 1,987 | -3.6 | 311 | 547 | 75.9 |
| Hawaii | 2.5 | 5,205 | 5,768 | 10.8 | 4,820 | 5,113 | 6.1 | 385 | 611 | 58.7 | NA | 44 | NA |
| Idaho | 2.3 | 6,619 | 6,287 | -5.0 | 6,467 | 6,125 | -5.3 | 137 | 148 | 8.0 | 15 | 14 | -6.7 |
| Illinois | 14.5 | 42,945 | 44,616 | 3.9 | 39,856 | 41,234 | 3.5 | 2,876 | 3,176 | 10.4 | 213 | 206 | -3.3 |
| Indiana | 7.0 | 28,288 | 25,465 | -10.0 | 27,466 | 23,861 | -13.1 | 531 | 930 | 75.1 | 291 | 674 | 131.6 |
| Iowa | 4.0 | 9,731 | 8,975 | -7.8 | 8,946 | 8,180 | -8.6 | 738 | 747 | 1.2 | 47 | 48 | 2.1 |
| Kansas | -1.5 | 10,863 | 11,471 | 5.6 | 9,916 | 10,603 | 6.9 | 935 | 834 | -10.8 | 12 | 34 | 183.3 |
| Kentucky | 16.5 | 24,071 | 23,565 | -2.1 | 21,175 | 20,697 | -2.3 | 2,509 | 2,347 | -6.5 | 387 | 521 | 34.6 |
| Louisiana | 4.8 | 9,903 | 12,011 | 21.3 | 8,241 | 9,930 | 20.5 | 1,464 | 1,765 | 20.6 | 198 | 316 | 59.6 |
| Maine | -5.4 | 11,373 | 10,849 | -4.6 | 10,865 | 10,483 | -3.5 | 362 | 289 | -20.2 | 146 | 77 | -47.3 |
| Maryland | 14.0 | 42,128 | 46,913 | 11.4 | 39,992 | 44,659 | 11.7 | 1,704 | 1,989 | 16.7 | 432 | 265 | -38.7 |
| Massachusetts | 12.8 | 44,133 | 45,438 | 3.0 | 40,227 | 40,734 | 1.3 | 3,171 | 3,602 | 13.6 | 735 | 1,102 | 49.9 |
| Michigan | 23.0 | 47,749 | 46,781 | -2.0 | 42,045 | 43,577 | 3.6 | 5,241 | 3,043 | -41.9 | 463 | 161 | -65.2 |
| Minnesota | 7.0 | 18,034 | 19,235 | 6.7 | 14,223 | 15,676 | 10.2 | 3,753 | 3,487 | -7.1 | 58 | 72 | 24.1 |
| Mississippi | 0.6 | 6,726 | 4,699 | -30.1 | 5,360 | 3,547 | -33.8 | 994 | 841 | -15.4 | 372 | 311 | -16.4 |
| Missouri | -17.1 | 23,028 | 25,015 | 8.6 | 21,600 | 22,590 | 4.6 | 1,279 | 2,223 | 73.8 | 149 | 202 | 35.6 |
| Montana | 17.9 | 4,429 | 5,064 | 14.3 | 3,809 | 4,785 | 25.6 | 488 | 187 | -61.7 | 132 | 92 | -30.3 |
| Nebraska | 1.6 | 6,374 | 5,735 | -10.0 | 5,690 | 4,909 | -13.7 | 684 | 824 | 20.5 | NA | 2 | NA |
| Nevada | 42.0 | 7,048 | 6,930 | -1.7 | 6,403 | 6,179 | -3.5 | 492 | 487 | -1.0 | 153 | 264 | 72.5 |
| New Hampshire | 30.1 | 6,702 | 8,164 | 21.8 | 6,326 | 7,766 | 22.8 | 367 | 394 | 7.4 | 9 | 4 | -55.6 |
| New Jersey | 26.1 | 36,605 | 36,708 | 0.3 | 33,068 | 32,578 | -1.5 | 2,813 | 3,404 | 21.0 | 724 | 726 | 0.3 |
| New Mexico | 15.7 | 12,868 | 15,062 | 17.1 | 10,949 | 14,499 | 32.4 | 1,808 | 449 | -75.2 | 111 | 114 | 2.7 |
| New York | 9.7 | 114,660 | 113,713 | -0.8 | 103,167 | 101,982 | -1.1 | 9,839 | 9,986 | 1.5 | 1,654 | 1,745 | 5.5 |
| North Carolina | 3.2 | 40,575 | 42,026 | 3.6 | 37,394 | 38,374 | 2.6 | 2,481 | 3,196 | 28.8 | 700 | 456 | -34.9 |
| North Dakota | 9.0 | 1,785 | 2,404 | 34.7 | 1,222 | 1,949 | 59.5 | 510 | 396 | -22.4 | 53 | 59 | 11.3 |
| Ohio | 25.2 | 37,262 | 45,129 | 21.1 | 34,397 | 42,006 | 22.1 | 2,365 | 2,406 | 1.7 | 500 | 717 | 43.4 |
| Oklahoma | 0.6 | 16,700 | 16,783 | 0.5 | 15,356 | 15,512 | 1.0 | 1,204 | 1,171 | -2.7 | 140 | 100 | -28.6 |
| Oregon | 25.0 | 21,898 | 30,401 | 38.8 | 20,537 | 29,047 | 41.4 | 1,299 | 1,258 | -3.2 | 62 | 96 | 54.8 |
| Pennsylvania | 4.1 | 57,715 | 59,584 | 3.2 | 52,011 | 53,822 | 3.5 | 5,245 | 5,433 | 3.6 | 459 | 329 | -28.3 |
| Puerto Rico | NA | 15,169 | 11,358 | -25.1 | 12,119 | 7,817 | -35.5 | 2,511 | 2,971 | 18.3 | 539 | 570 | 5.8 |
| Rhode Island | 23.2 | 10,404 | 14,269 | 37.1 | 10,039 | 9,005 | -10.3 | 323 | 1,723 | 433.4 | 42 | 3,541 | 8,331.0 |
| South Carolina | -2.8 | 15,824 | 18,236 | 15.2 | 14,906 | 16,473 | 10.5 | 552 | 614 | 11.2 | 366 | 1,149 | 213.9 |
| South Dakota | 2.5 | 3,267 | 2,964 | -9.3 | 2,569 | 2,308 | -10.2 | 623 | 585 | -6.1 | 75 | 71 | -5.3 |
| Tennessee | 13.4 | 14,149 | 22,445 | 58.6 | 11,698 | 20,187 | 72.6 | 2,010 | 1,994 | -0.8 | 441 | 264 | -40.1 |
| Texas | 6.3 | 34,704 | 35,293 | 1.7 | 28,843 | 26,984 | -6.4 | 5,065 | 6,391 | 26.2 | 796 | 1,918 | 141.0 |
| Utah | 0.5 | 12,586 | 12,496 | -0.7 | 11,183 | 11,070 | -1.0 | 1,389 | 1,379 | -0.7 | 14 | 47 | 235.7 |
| Vermont | 8.2 | 5,230 | 7,380 | 41.1 | 4,124 | 6,522 | 58.1 | 1,013 | 164 | -83.8 | 93 | 694 | 646.2 |
| Virginia | -6.8 | 22,838 | 22,305 | -2.3 | 21,879 | 20,807 | -4.9 | 712 | 1,174 | 64.9 | 247 | 324 | 31.2 |
| Washington | 24.2 | 42,030 | 50,633 | 20.5 | 39,680 | 43,724 | 10.2 | 2,210 | 6,762 | 206.0 | 140 | 147 | 5.0 |
| West Virginia | 14.8 | 10,057 | 10,099 | 0.4 | 9,547 | 9,500 | -0.5 | 492 | 545 | 10.8 | 18 | 54 | 200.0 |
| Wisconsin | -10.4 | 28,657 | 24,371 | -15.0 | 26,314 | 23,235 | -11.7 | 2,068 | 888 | -57.1 | 275 | 248 | -9.8 |
| Wyoming | -2.6 | 2,798 | 3,261 | 16.5 | 2,465 | 2,916 | 18.3 | 326 | 331 | 1.5 | 7 | 14 | 100.0 |
| U.S. territories | NA | 314 | 315 | 0.3 | 260 | 248 | -4.6 | 51 | 43 | -15.7 | 3 | 24 | 700.0 |
| SOURCE: N-SSATS 2013 and 2015. NOTE: Inpatient and residential client counts represent the number of clients receiving services on March 31 of the indicated year (see Questions 28a and 29a in N-SSATS 2013 and Questions 29a and 30a in N-SSATS 2015). Outpatient client counts represent the number of clients who received outpatient services in March of the indicated year and who were still enrolled in care at the facility where they received those services on March 31 (see Question 30a in N-SSATS 2013 and Question 31a in N-SSATS 2015). Total clients is the sum of inpatient, residential, and outpatient clients.
|
|||||||||||||
| TABLE B.3.a. Number of Clients Receiving Medications by Geographic Location and Facility Characteristics, 2013 and 2015 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Receiving Methadone | Receiving Buprenorphine | Receiving Injectable Naltrexone | |||||||||
| 2013 | 2015 | % Change | 2013 | 2015 | % Change | 2013 | 2015 | % Change | 2013 | 2015 | % Change | |
| Total | 382,237 | 439,602 | 15 | 330,308 | 356,843 | 8 | 48,148 | 75,724 | 57 | 3,781 | 7,035 | 86 |
| States in which Medicaid enrollment increased more than 10% between January 2014 and January 2015 | ||||||||||||
| Yes | 166,201 | 206,158 | 24 | 140,659 | 166,890 | 19 | 24,043 | 35,575 | 48 | 1,499 | 3,693 | 146 |
| No | 208,168 | 228,187 | 10 | 182,208 | 185,422 | 2 | 23,711 | 39,436 | 66 | 2,249 | 3,329 | 48 |
| Region | ||||||||||||
| Northeast | 128,212 | 138,585 | 8 | 112,198 | 114,087 | 1 | 15,093 | 22,620 | 50 | 921 | 1,878 | 104 |
| Midwest | 57,894 | 71,447 | 23 | 48,286 | 53,687 | 11 | 8,539 | 15,579 | 82 | 1,069 | 2,181 | 104 |
| South | 121,655 | 145,753 | 20 | 103,161 | 116,555 | 13 | 17,441 | 27,649 | 59 | 1,053 | 1,549 | 47 |
| West | 65,682 | 78,560 | 19 | 58,296 | 67,983 | 16 | 6,681 | 9,163 | 37 | 705 | 1,414 | 101 |
| Urbanicity | ||||||||||||
| Urban | 304,932 | 403,601 | 32 | 265,239 | 332,937 | 26 | 36,896 | 64,372 | 74 | 2,797 | 6,292 | 125 |
| Rural | 68,511 | 30,744 | -55 | 56,702 | 19,375 | -66 | 10,858 | 10,639 | -2 | 951 | 730 | -23 |
| Facility focus | ||||||||||||
| SUD treatment | NA | 376,265 | NA | NA | 327,936 | NA | NA | 44,616 | NA | NA | 3,713 | NA |
| MH treatment | NA | 4,233 | NA | NA | 1,416 | NA | NA | 2,568 | NA | NA | 249 | NA |
| SUD and MH treatment | NA | 45,718 | NA | NA | 18,244 | NA | NA | 24,671 | NA | NA | 2,803 | NA |
| Other | NA | 13,386 | NA | NA | 9,247 | NA | NA | 3,869 | NA | NA | 270 | NA |
| Operation | ||||||||||||
| Private, NP | 130,181 | 153,994 | 18 | 111,313 | 121,499 | 9 | 17,610 | 29,149 | 66 | 1,258 | 3,346 | 166 |
| Private, FP | 214,533 | 252,423 | 18 | 189,264 | 213,421 | 13 | 23,152 | 36,286 | 57 | 2,117 | 2,716 | 28 |
| Public | 37,523 | 33,185 | -12 | 29,731 | 21,923 | -26 | 7,386 | 10,289 | 39 | 406 | 973 | 140 |
| SOURCE: N-SSATS 2013 and 2015. NOTE: The number of clients receiving methadone, buprenorphine, or injectable naltrexone is based on counts of clients receiving these services as reported in Questions 28c, 29c, and 30c in N-SSATS 2013 and Questions 29c, 30c, and 31c in N-SSATS 2015. Total clients is the sum of methadone, buprenorphine, or injectable naltrexone clients. United States territories are excluded from the categories for: (1) region; and (2) states in which Medicaid enrollment increased more than 10% between January 2014 and January 2015. The percent increase in Medicaid enrollment for each state was determined based on Medicaid enrollment reports. Therefore, the totals for these categories are lower than the reported total in the first line of the table. Urbanicity is assigned based on the National Center for Health Statistics urbanicity classification scheme. Facilities in rural areas include those in micropolitan areas with an urban core population of at least 10,000 but less than 50,000, as well as those in non-core areas. Facilities in a central or fringe urban core with a population of 50,000 or more are considered urban. Information on urbanicity was not available for all facilities; urban and rural client counts are only reported for facilities with known urbanicity. Facility operation was self-designated in N-SSATS Question 4 in 2013 and Question 7 in 2015. Facility focus was not asked on the N-SSATS 2013 survey. |
||||||||||||
| TABLE B.3.b. Proportion of Clients Receiving Medications by Geographic Location, 2013 and 2015 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Receiving Methadone | Receiving Buprenorphine | Receiving Injectable Naltrexone | |||||||||
| 2013 | 2015 | % Change | 2013 | 2015 | % Change | 2013 | 2015 | % Change | 2013 | 2015 | % Change | |
| Total | 31 | 34 | 10 | 26 | 27 | 3 | 4 | 6 | 51 | 0 | 1 | 78 |
| States in which Medicaid enrollment increased more than 10% between January 2014 and January 2015 | ||||||||||||
| Yes | 28 | 33 | 17 | 24 | 26 | 12 | 4 | 6 | 39 | 0 | 1 | 132 |
| No | 33 | 35 | 6 | 29 | 28 | -2 | 4 | 6 | 61 | 0 | 1 | 43 |
| Region | ||||||||||||
| Northeast | 40 | 42 | 4 | 35 | 34 | -3 | 5 | 7 | 44 | 0 | 1 | 95 |
| Midwest | 22 | 27 | 21 | 19 | 20 | 9 | 3 | 6 | 80 | 0 | 1 | 101 |
| South | 35 | 39 | 10 | 30 | 31 | 3 | 5 | 7 | 45 | 0 | 0 | 34 |
| West | 21 | 25 | 16 | 19 | 21 | 13 | 2 | 3 | 33 | 0 | 0 | 95 |
| Urbanicity | ||||||||||||
| Urban | 32 | 37 | 15 | 28 | 30 | 9 | 4 | 6 | 51 | 0 | 1 | 95 |
| Rural | 25 | 16 | -34 | 20 | 10 | -50 | 4 | 6 | 44 | 0 | 0 | 13 |
| Operation | ||||||||||||
| Private, NP | 20 | 23 | 13 | 17 | 18 | 4 | 3 | 4 | 58 | 0 | 0 | 153 |
| Private, FP | 50 | 53 | 6 | 44 | 45 | 2 | 5 | 8 | 42 | 0 | 1 | 16 |
| Public | 21 | 21 | 0 | 16 | 14 | -17 | 4 | 6 | 58 | 0 | 1 | 171 |
| SOURCE: N-SSATS 2013 and 2015. NOTE: The percentage of clients receiving methadone, buprenorphine, or injectable naltrexone is based on counts of clients receiving these services (as reported in Table B.3.a) divided by the total number of clients (indicated in Table B.1). United States territories are excluded from the categories for: (1) region; and (2) states in which Medicaid enrollment increased more than 10% between January 2014 and January 2015. The percent increase in Medicaid enrollment for each state was determined based on Medicaid enrollment reports. Urbanicity is assigned based on the National Center for Health Statistics urbanicity classification scheme. Facilities in rural areas include those in micropolitan areas with an urban core population of at least 10,000 but less than 50,000, as well as those in non-core areas. Facilities in a central or fringe urban core with a population of 50,000 or more are considered urban. Information on urbanicity was not available for all facilities; urban and rural estimates are only reported for facilities with known urbanicity. Facility operation was self-designated in N-SSATS Question 4 in 2013 and Question 7 in 2015. |
||||||||||||
| TABLE B.4.a. Number of Clients Receiving Medications by State, 2013 and 2015 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Receiving Methadone | Receiving Buprenorphine | Receiving Injectable Naltrexone | |||||||||
| 2013 | 2015 | % Change | 2013 | 2015 | % Change | 2013 | 2015 | % Change | 2013 | 2015 | % Change | |
| Total | 383,130 | 439,602 | 15 | 331,215 | 356,843 | 8 | 48,134 | 75,724 | 57 | 3,781 | 7,035 | 86 |
| Alabama | 8,785 | 8,457 | -4 | 7,738 | 7,639 | -1 | 967 | 787 | -19 | 80 | 31 | -61 |
| Alaska | 285 | 444 | 56 | 144 | 331 | 130 | 137 | 91 | -34 | 4 | 22 | 450 |
| Arizona | 7,585 | 8,291 | 9 | 6,425 | 7,107 | 11 | 1,040 | 987 | -5 | 120 | 197 | 64 |
| Arkansas | 992 | 1,484 | 50 | 831 | 1,095 | 32 | 161 | 389 | 142 | NA | NA | NA |
| California | 33,301 | 38,607 | 16 | 30,899 | 35,231 | 14 | 2,154 | 2,922 | 36 | 248 | 454 | 83 |
| Colorado | 2,561 | 2,290 | -11 | 2,084 | 1,934 | -7 | 379 | 256 | -32 | 98 | 100 | 2 |
| Connecticut | 16,540 | 14,658 | -11 | 15,531 | 14,072 | -9 | 980 | 544 | -44 | 29 | 42 | 45 |
| Delaware | 2,826 | 5,834 | 106 | 2,422 | 3,266 | 35 | 380 | 2,425 | 538 | 24 | 143 | 496 |
| District of Columbia | 1,856 | 1,428 | -23 | 1,760 | 1,315 | -25 | 93 | 104 | 12 | 3 | 9 | 200 |
| Florida | 16,471 | 20,978 | 27 | 14,441 | 17,670 | 22 | 1,700 | 2,922 | 72 | 330 | 386 | 17 |
| Georgia | 10,542 | 11,990 | 14 | 10,194 | 11,212 | 10 | 297 | 659 | 122 | 51 | 119 | 133 |
| Hawaii | 700 | 745 | 6 | 612 | 623 | 2 | 87 | 121 | 39 | 1 | 1 | 0 |
| Idaho | 147 | 678 | 361 | NA | 312 | NA | 137 | 353 | 158 | 10 | 13 | 30 |
| Illinois | 13,230 | 15,053 | 14 | 11,922 | 13,559 | 14 | 1,199 | 1,303 | 9 | 109 | 191 | 75 |
| Indiana | 10,037 | 8,393 | -16 | 9,265 | 7,073 | -24 | 744 | 1,178 | 58 | 28 | 142 | 407 |
| Iowa | 692 | 889 | 28 | 623 | 783 | 26 | 69 | 106 | 54 | NA | NA | NA |
| Kansas | 2,284 | 2,585 | 13 | 2,077 | 2,313 | 11 | 207 | 261 | 26 | NA | 11 | NA |
| Kentucky | 4,719 | 5,136 | 9 | 1,626 | 2,955 | 82 | 3,079 | 2,158 | -30 | 14 | 23 | 64 |
| Louisiana | 2,193 | 4,731 | 116 | 1,907 | 3,502 | 84 | 271 | 1,153 | 325 | 15 | 76 | 407 |
| Maine | 4,503 | 5,304 | 18 | 3,658 | 3,751 | 3 | 838 | 1,529 | 82 | 7 | 24 | 243 |
| Maryland | 22,278 | 26,692 | 20 | 19,564 | 22,927 | 17 | 2,622 | 3,533 | 35 | 92 | 232 | 152 |
| Massachusetts | 19,626 | 22,146 | 13 | 15,479 | 17,633 | 14 | 3,861 | 4,113 | 7 | 286 | 400 | 40 |
| Michigan | 9,116 | 12,064 | 32 | 7,851 | 9,806 | 25 | 1,187 | 1,900 | 60 | 78 | 358 | 359 |
| Minnesota | 5,048 | 6,258 | 24 | 4,533 | 5,530 | 22 | 483 | 667 | 38 | 32 | 61 | 91 |
| Mississippi | 257 | 274 | 7 | 183 | 176 | -4 | 70 | 97 | 39 | 4 | 1 | -75 |
| Missouri | 3,817 | 4,764 | 25 | 2,704 | 3,083 | 14 | 738 | 1,155 | 57 | 375 | 526 | 40 |
| Montana | 382 | 773 | 102 | 174 | 489 | 181 | 190 | 284 | 49 | 18 | NA | NA |
| Nebraska | 954 | 688 | -28 | 553 | 619 | 12 | 78 | 52 | -33 | 323 | 17 | -95 |
| Nevada | 1,572 | 1,847 | 17 | 1,493 | 1,555 | 4 | 75 | 261 | 248 | 4 | 31 | 675 |
| New Hampshire | 2,656 | 4,754 | 79 | 2,340 | 2,748 | 17 | 311 | 1,991 | 540 | 5 | 15 | 200 |
| New Jersey | 12,818 | 14,506 | 13 | 11,704 | 13,103 | 12 | 1,036 | 1,166 | 13 | 78 | 237 | 204 |
| New Mexico | 2,752 | 5,029 | 83 | 2,407 | 4,088 | 70 | 332 | 890 | 168 | 13 | 51 | 292 |
| New York | 43,740 | 41,502 | -5 | 38,873 | 34,535 | -11 | 4,540 | 6,394 | 41 | 327 | 573 | 75 |
| North Carolina | 14,930 | 19,382 | 30 | 11,499 | 13,665 | 19 | 3,369 | 5,637 | 67 | 62 | 80 | 29 |
| North Dakota | 9 | 109 | 1,111 | NA | NA | NA | 9 | 84 | 833 | NA | 25 | NA |
| Ohio | 7,580 | 14,092 | 86 | 4,908 | 6,147 | 25 | 2,618 | 7,347 | 181 | 54 | 598 | 1,007 |
| Oklahoma | 3,279 | 3,760 | 15 | 3,091 | 3,500 | 13 | 188 | 227 | 21 | NA | 33 | NA |
| Oregon | 4,348 | 5,322 | 22 | 4,045 | 4,663 | 15 | 288 | 601 | 109 | 15 | 58 | 287 |
| Pennsylvania | 23,096 | 24,262 | 5 | 20,623 | 20,408 | -1 | 2,308 | 3,530 | 53 | 165 | 324 | 96 |
| Puerto Rico | 8,761 | 5,230 | -40 | 8,348 | 4,515 | -46 | 380 | 702 | 85 | 33 | 13 | -61 |
| Rhode Island | 4,243 | 7,552 | 78 | 3,517 | 6,213 | 77 | 715 | 1,078 | 51 | 11 | 261 | 2,273 |
| South Carolina | 5,020 | 5,334 | 6 | 4,323 | 4,524 | 5 | 671 | 799 | 19 | 26 | 11 | -58 |
| South Dakota | 83 | 10 | -88 | 82 | 5 | -94 | 1 | 5 | 400 | NA | NA | NA |
| Tennessee | 2,974 | 5,721 | 92 | 2,427 | 4,421 | 82 | 488 | 1,179 | 142 | 59 | 121 | 105 |
| Texas | 12,497 | 12,126 | -3 | 11,662 | 9,833 | -16 | 673 | 2,189 | 225 | 162 | 104 | -36 |
| Utah | 3,028 | 3,489 | 15 | 2,635 | 2,459 | -7 | 345 | 790 | 129 | 48 | 240 | 400 |
| Vermont | 1,435 | 3,901 | 172 | 918 | 1,624 | 77 | 504 | 2,275 | 351 | 13 | 2 | -85 |
| Virginia | 6,655 | 7,096 | 7 | 5,323 | 5,735 | 8 | 1,278 | 1,319 | 3 | 54 | 42 | -22 |
| Washington | 8,950 | 10,953 | 22 | 7,495 | 9,191 | 23 | 1,335 | 1,534 | 15 | 120 | 228 | 90 |
| West Virginia | 5,510 | 5,330 | -3 | 4,299 | 3,120 | -27 | 1,134 | 2,072 | 83 | 77 | 138 | 79 |
| Wisconsin | 5,279 | 6,542 | 24 | 4,003 | 4,769 | 19 | 1,206 | 1,521 | 26 | 70 | 252 | 260 |
| Wyoming | 188 | 92 | -51 | NA | NA | NA | 182 | 73 | -60 | 6 | 19 | 217 |
| SOURCE: N-SSATS 2013 and 2015. NOTE: The number of clients receiving methadone, buprenorphine, or injectable naltrexone is based on counts of clients receiving these services, as reported in Questions 28c, 29c, and 30c in N-SSATS 2013 and Questions 29c, 30c, and 31c in N-SSATS 2015. Total clients is the sum of methadone, buprenorphine, or injectable naltrexone clients. |
||||||||||||
| TABLE B.4.b. Proportion of Clients Receiving Medications by State, 2013 and 2015 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Receiving Methadone | Receiving Buprenorphine | Receiving Injectable Naltrexone | |||||||||
| 2013 | 2015 | % Change | 2013 | 2015 | % Change | 2013 | 2015 | % Change | 2013 | 2015 | % Change | |
| Total | 31 | 34 | 10 | 27 | 27 | 3 | 4 | 6 | 51 | 0 | 1 | 78 |
| Alabama | 58 | 58 | 0 | 51 | 53 | 2 | 6 | 5 | -16 | 1 | 0 | -60 |
| Alaska | 7 | 13 | 81 | 4 | 10 | 167 | 4 | 3 | -23 | 0 | 1 | 538 |
| Arizona | 24 | 24 | 2 | 20 | 21 | 4 | 3 | 3 | -11 | 0 | 1 | 54 |
| Arkansas | 17 | 21 | 24 | 14 | 15 | 9 | 3 | 5 | 100 | 0 | 0 | NA |
| California | 28 | 34 | 21 | 26 | 31 | 19 | 2 | 3 | 42 | 0 | 0 | 92 |
| Colorado | 6 | 7 | 9 | 5 | 6 | 13 | 1 | 1 | -18 | 0 | 0 | 24 |
| Connecticut | 50 | 39 | -22 | 47 | 37 | -20 | 3 | 1 | -51 | 0 | 0 | 27 |
| Delaware | 54 | 56 | 6 | 46 | 32 | -31 | 7 | 23 | 226 | 0 | 1 | 205 |
| District of Columbia | 48 | 51 | 4 | 46 | 47 | 1 | 2 | 4 | 52 | 0 | 0 | 307 |
| Florida | 31 | 33 | 8 | 27 | 28 | 4 | 3 | 5 | 46 | 1 | 1 | -1 |
| Georgia | 44 | 47 | 8 | 42 | 44 | 4 | 1 | 3 | 110 | 0 | 0 | 121 |
| Hawaii | 13 | 13 | -4 | 12 | 11 | -8 | 2 | 2 | 26 | 0 | 0 | -10 |
| Idaho | 2 | 11 | 386 | NA | 5 | NA | 2 | 6 | 171 | 0 | 0 | 37 |
| Illinois | 31 | 34 | 10 | 28 | 30 | 9 | 3 | 3 | 5 | 0 | 0 | 69 |
| Indiana | 35 | 33 | -7 | 33 | 28 | -15 | 3 | 5 | 76 | 0 | 1 | 463 |
| Iowa | 7 | 10 | 39 | 6 | 9 | 36 | 1 | 1 | 67 | NA | NA | NA |
| Kansas | 21 | 23 | 7 | 19 | 20 | 5 | 2 | 2 | 19 | NA | 0 | NA |
| Kentucky | 20 | 22 | 11 | 7 | 13 | 86 | 13 | 9 | -28 | 0 | 0 | 68 |
| Louisiana | 22 | 39 | 78 | 19 | 29 | 51 | 3 | 10 | 251 | 0 | 1 | 318 |
| Maine | 40 | 49 | 23 | 32 | 35 | 7 | 7 | 14 | 91 | 0 | 0 | 259 |
| Maryland | 53 | 57 | 8 | 46 | 49 | 5 | 6 | 8 | 21 | 0 | 0 | 126 |
| Massachusetts | 44 | 49 | 10 | 35 | 39 | 11 | 9 | 9 | 3 | 1 | 1 | 36 |
| Michigan | 19 | 26 | 35 | 16 | 21 | 27 | 2 | 4 | 63 | 0 | 1 | 368 |
| Minnesota | 28 | 33 | 16 | 25 | 29 | 14 | 3 | 3 | 29 | 0 | 0 | 79 |
| Mississippi | 4 | 6 | 53 | 3 | 4 | 38 | 1 | 2 | 98 | 0 | 0 | -64 |
| Missouri | 17 | 19 | 15 | 12 | 12 | 5 | 3 | 5 | 44 | 2 | 2 | 29 |
| Montana | 9 | 15 | 77 | 4 | 10 | 146 | 4 | 6 | 31 | 0 | NA | NA |
| Nebraska | 15 | 12 | -20 | 9 | 11 | 24 | 1 | 1 | -26 | 5 | 0 | -94 |
| Nevada | 22 | 27 | 19 | 21 | 22 | 6 | 1 | 4 | 254 | 0 | 0 | 688 |
| New Hampshire | 40 | 58 | 47 | 35 | 34 | -4 | 5 | 24 | 426 | 0 | 0 | 146 |
| New Jersey | 35 | 40 | 13 | 32 | 36 | 12 | 3 | 3 | 12 | 0 | 1 | 203 |
| New Mexico | 21 | 33 | 56 | 19 | 27 | 45 | 3 | 6 | 129 | 0 | 0 | 235 |
| New York | 38 | 36 | -4 | 34 | 30 | -10 | 4 | 6 | 42 | 0 | 1 | 77 |
| North Carolina | 37 | 46 | 25 | 28 | 33 | 15 | 8 | 13 | 62 | 0 | 0 | 25 |
| North Dakota | 1 | 5 | 799 | NA | NA | NA | 1 | 3 | 593 | NA | 1 | NA |
| Ohio | 20 | 31 | 54 | 13 | 14 | 3 | 7 | 16 | 132 | 0 | 1 | 814 |
| Oklahoma | 20 | 22 | 14 | 19 | 21 | 13 | 1 | 1 | 20 | NA | 0 | NA |
| Oregon | 20 | 18 | -12 | 18 | 15 | -17 | 1 | 2 | 50 | 0 | 0 | 179 |
| Pennsylvania | 40 | 41 | 2 | 36 | 34 | -4 | 4 | 6 | 48 | 0 | 1 | 90 |
| Puerto Rico | 58 | 46 | -20 | 55 | 40 | -28 | 3 | 6 | 147 | 0 | 0 | -47 |
| Rhode Island | 41 | 53 | 30 | 34 | 44 | 29 | 7 | 8 | 10 | 0 | 2 | 1,630 |
| South Carolina | 32 | 29 | -8 | 27 | 25 | -9 | 4 | 4 | 3 | 0 | 0 | -63 |
| South Dakota | 3 | 0 | -87 | 3 | 0 | -93 | 0 | 0 | 451 | NA | NA | NA |
| Tennessee | 21 | 25 | 21 | 17 | 20 | 15 | 3 | 5 | 52 | 0 | 1 | 29 |
| Texas | 36 | 34 | -5 | 34 | 28 | -17 | 2 | 6 | 220 | 0 | 0 | -37 |
| Utah | 24 | 28 | 16 | 21 | 20 | -6 | 3 | 6 | 131 | 0 | 2 | 404 |
| Vermont | 27 | 53 | 93 | 18 | 22 | 25 | 10 | 31 | 220 | 0 | 0 | -89 |
| Virginia | 29 | 32 | 9 | 23 | 26 | 10 | 6 | 6 | 6 | 0 | 0 | -20 |
| Washington | 21 | 22 | 2 | 18 | 18 | 2 | 3 | 3 | -5 | 0 | 0 | 58 |
| West Virginia | 55 | 53 | -4 | 43 | 31 | -28 | 11 | 21 | 82 | 1 | 1 | 78 |
| Wisconsin | 18 | 27 | 46 | 14 | 20 | 40 | 4 | 6 | 48 | 0 | 1 | 323 |
| Wyoming | 7 | 3 | -58 | NA | NA | NA | 7 | 2 | -66 | 0 | 1 | 172 |
| SOURCE: N-SSATS 2013 and 2015. NOTE: The percentage of clients receiving methadone, buprenorphine, or injectable naltrexone is based on counts of clients receiving these services (as reported in Table B.2) relative to the total number of clients (indicated in Table B.4.a). |
||||||||||||
| TABLE B.5. Substance Dependence or Abuse for Specific Substances in the Past Year Among Persons Age 12 or Older, 2002-2015 | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Past Year Dependence or Abuse | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 |
| Illicit drugsa | 7,116 | 6,835 | 7,298 | 6,833 | 7,024 | 6,866 | 7,012 | 7,114 | 7,144 | 6,531 | 7,312 | 6,852 | 7,077 | 7,737n |
| Marijuana and hashish | 4,294 | 4,198 | 4,469 | 4,090 | 4,184 | 3,941 | 4,228 | 4,322 | 4,505 | 4,165 | 4,304 | 4,206 | 4,176 | 4,007 |
| Cocaine | 1,488** | 1,515** | 1,571** | 1,549** | 1,665** | 1,604** | 1,412** | 1,108 | 1,012 | 821 | 1,119 | 855 | 913 | 896 |
| Heroin | 214** | 189** | 270** | 227** | 324** | 214** | 283** | 369* | 361** | 426 | 467 | 517 | 586 | 591 |
| Hallucinogens | 426** | 321 | 449** | 371* | 380* | 369* | 362* | 373* | 402** | 342 | 331 | 277 | 246 | 267n |
| Inhalants | 180* | 169* | 233** | 221** | 176* | 164* | 175* | 164* | 169* | 141 | 164 | 132 | 96 | 121n |
| Non-medical use of psychotherapeuticsb,c | 2,018* | 1,923** | 2,048* | 1,959** | 2,036* | 2,167 | 2,177 | 2,297 | 2,378 | 2,139 | 2,597 | 2,281 | 2,417 | 2,742n |
| Pain relievers | 1,509* | 1,424** | 1,388** | 1,546* | 1,636 | 1,715 | 1,715 | 1,878 | 1,923 | 1,768 | 2,056 | 1,879 | 1,918 | 2,038n |
| Tranquilizers | 509 | 435 | 573 | 419 | 403 | 443 | 453 | 476 | 522 | 400 | 629 | 423 | 472 | 688n |
| Stimulantsb | 436 | 378 | 470 | 409 | 388 | 405 | 351 | 380 | 358 | 329* | 535 | 469 | 476 | 426n |
| Sedatives | 154 | 158 | 128 | 97 | 121 | 154 | 127 | 147 | 162 | 78 | 135 | 99 | 143 | 154n |
| Alcohol | 18,100* | 17,805 | 18,654** | 18,658** | 18,852** | 18,687** | 18,478** | 18,763** | 17,967 | 16,672 | 17,714 | 17,298 | 16,994 | 15,736 |
| Both illicit drugs and alcohola | 3,210** | 3,054* | 3,445** | 3,273** | 3,215** | 3,184** | 3,102** | 3,243** | 2,889 | 2,598 | 2,840 | 2,589 | 2,592 | 2,663n |
| Illicit drugs or alcohola | 22,006 | 21,586 | 22,506 | 22,218 | 22,661* | 22,369 | 22,388 | 22,634 | 22,221 | 20,605 | 22,187 | 21,561 | 21,480 | 20,810n |
| SOURCE: Results for 2002 to 2014 are extracted from Table 7.50A in Center for Behavioral Health Statistics and Quality 2015. Results for 2015 are extracted from Table 7.40A in the Center for Behavioral Health Statistics and Quality 2016. NOTE: Dependence or abuse is based on definitions found in the fourth edition of the DSM. a. Illicit drugs include marijuana and hashish, cocaine (including crack), heroin, hallucinogens, inhalants, and prescription psychotherapeutics used non-medically including data from original NSDUH questions regarding methamphetamines but not new items added in 2005 and 2006 NSDUH. b. Estimates in these designated rows do not include data from new methamphetamine items added in 2005 and 2006. c. Non-medical use of prescription psychotherapeutics includes the non-medical use of pain relievers, tranquilizers, stimulants, or sedatives and does not include over-the-counter drugs. n. Estimates are not comparable to prior years due to changes in the survey methodology. *The difference between this estimate and the 2014 estimate is statistically significant at the 0.05 level. **The difference between this estimate and the 2014 estimate is statistically significant at the 0.01 level. |
||||||||||||||
| TABLE B.6. Proportion of Individuals 12 or Older Reporting Symptoms of SUD but Not Receiving Any Treatment, by State, 2013-2014 | ||||||
|---|---|---|---|---|---|---|
| Drug Use Disorders | Alcohol Use Disorders | |||||
| With a Disorder (thousands) |
With a Disorder but Not Receiving Treatment |
With a Disorder (thousands) |
With a Disorder but Not Receiving Treatment |
|||
| Number (thousands) |
Percentage | Number (thousands) |
Percentage | |||
| Total | 6,964 | 6,202 | 89 | 17,147 | 16,351 | 95 |
| Alabama | 107 | 98 | 92 | 233 | 225 | 97 |
| Alaska | 19 | 16 | 84 | 39 | 37 | 95 |
| Arizona | 177 | 157 | 89 | 418 | 383 | 92 |
| Arkansas | 58 | 53 | 91 | 128 | 126 | 98 |
| California | 876 | 791 | 90 | 2,127 | 2,030 | 95 |
| Colorado | 128 | 113 | 88 | 329 | 304 | 92 |
| Connecticut | 88 | 75 | 85 | 206 | 199 | 97 |
| Delaware | 27 | 20 | 74 | 48 | 46 | 96 |
| District of Columbia | 20 | 18 | 90 | 55 | 52 | 95 |
| Florida | 410 | 369 | 90 | 1,008 | 976 | 97 |
| Georgia | 238 | 208 | 87 | 506 | 482 | 95 |
| Hawaii | 26 | 25 | 96 | 78 | 73 | 94 |
| Idaho | 31 | 28 | 90 | 88 | 83 | 94 |
| Illinois | 267 | 246 | 92 | 661 | 636 | 96 |
| Indiana | 155 | 132 | 85 | 364 | 347 | 95 |
| Iowa | 56 | 52 | 93 | 160 | 154 | 96 |
| Kansas | 55 | 49 | 89 | 174 | 166 | 95 |
| Kentucky | 96 | 82 | 85 | 202 | 200 | 99 |
| Louisiana | 112 | 96 | 86 | 228 | 222 | 97 |
| Maine | 30 | 26 | 87 | 65 | 64 | 98 |
| Maryland | 140 | 123 | 88 | 331 | 311 | 94 |
| Massachusetts | 173 | 156 | 90 | 383 | 361 | 94 |
| Michigan | 205 | 181 | 88 | 510 | 497 | 97 |
| Minnesota | 107 | 97 | 91 | 286 | 274 | 96 |
| Mississippi | 65 | 59 | 91 | 141 | 138 | 98 |
| Missouri | 129 | 112 | 87 | 320 | 310 | 97 |
| Montana | 18 | 17 | 94 | 65 | 59 | 91 |
| Nebraska | 37 | 33 | 89 | 115 | 110 | 96 |
| Nevada | 62 | 55 | 89 | 158 | 150 | 95 |
| New Hampshire | 32 | 27 | 84 | 87 | 83 | 95 |
| New Jersey | 178 | 160 | 90 | 486 | 459 | 94 |
| New Mexico | 51 | 44 | 86 | 118 | 113 | 96 |
| New York | 483 | 420 | 87 | 1,101 | 1,014 | 92 |
| North Carolina | 229 | 201 | 88 | 501 | 476 | 95 |
| North Dakota | 14 | 12 | 86 | 47 | 44 | 94 |
| Ohio | 267 | 229 | 86 | 646 | 619 | 96 |
| Oklahoma | 74 | 64 | 86 | 200 | 183 | 92 |
| Oregon | 99 | 89 | 90 | 233 | 217 | 93 |
| Pennsylvania | 297 | 253 | 85 | 717 | 684 | 95 |
| Rhode Island | 30 | 26 | 87 | 69 | 64 | 93 |
| South Carolina | 102 | 89 | 87 | 235 | 229 | 97 |
| South Dakota | 15 | 13 | 87 | 53 | 47 | 89 |
| Tennessee | 125 | 116 | 93 | 293 | 290 | 99 |
| Texas | 464 | 441 | 95 | 1,396 | 1,358 | 97 |
| Utah | 61 | 55 | 90 | 124 | 118 | 95 |
| Vermont | 17 | 14 | 82 | 39 | 36 | 92 |
| Virginia | 171 | 154 | 90 | 484 | 464 | 96 |
| Washington | 159 | 141 | 89 | 383 | 355 | 93 |
| West Virginia | 46 | 42 | 91 | 100 | 92 | 92 |
| Wisconsin | 126 | 112 | 89 | 376 | 356 | 95 |
| Wyoming | 11 | 9 | 82 | 36 | 35 | 97 |
| SOURCE: Data were extracted from "2013-2014 National Surveys on Drug Use and Health: Model-Based Estimated Totals" (CBHSQ 2015) as follows: number of individuals with illicit drug disorder in past year from Table 18, number of individuals with alcohol use disorder from Table 16, number with an illicit drug use disorder not receiving treatment from Table 21, and number with an alcohol use disorder not receiving treatment from Table 22. The authors calculated the percentage not receiving treatment by dividing the number of individuals with a disorder not receiving treatment by the total number of individuals with a disorder. | ||||||
| TABLE B.7. Total Paid Staff Working in Specialty SUD Treatment Facilities in the United States, by Profession, 2016 | |||||
|---|---|---|---|---|---|
| Profession | Total Staff Members | Total FTEsa | Percentage Certified in Addiction Treatment |
||
| Number | Percentage | Number | Percentage | ||
| Total | 256,449 | 100 | 197,559 | 100 | 27 |
| Medical staff | 55,665 | 22 | 37,317 | 19 | 19 |
| Physician | 14,811 | 6 | 7,576 | 4 | 42 |
| Pharmacist | 2,016 | 1 | 1,110 | 1 | 23 |
| Registered nurse | 22,238 | 9 | 16,515 | 8 | 8 |
| Licensed practical nurse | 10,316 | 4 | 8,073 | 4 | 10 |
| Mid-level medical personnel | 6,284 | 2 | 4,043 | 2 | 20 |
| Counseling staff | 104,742 | 41 | 83,776 | 42 | 45 |
| Doctoral-level counselor | 5,534 | 2 | 3,944 | 2 | 34 |
| Master's-level counselor | 54,629 | 21 | 43,267 | 22 | 40 |
| Bachelor's degree counselor | 26,447 | 10 | 22,038 | 11 | 49 |
| Associate's degree or no-degree counselor | 18,132 | 7 | 14,527 | 7 | 59 |
| Non-administrative support staff | 54,988 | 21 | 41,009 | 21 | 17 |
| Pharmacy assistant | 834 | <1 | 684 | <1 | 6 |
| Peer support staff | 11,523 | 4 | 8,877 | 4 | 21 |
| Care manager or patient navigator | 10,741 | 4 | 9,318 | 5 | 18 |
| Other recovery support worker | 18,236 | 7 | 14,233 | 7 | 12 |
| Interns, contractors or per diem staff, and intake coordinators | 11,504 | 4 | 6,402 | 3 | 20 |
| Other clinical staff | 2,150 | 1 | 1,495 | 1 | 32 |
| Administrative support staff | 41,054 | 16 | 35,457 | 18 | 7 |
SOURCE: N-SSATS 2016, Question 22.
|
|||||
| TABLE B.8. Total Unpaid Staff Working in Specialty SUD Treatment Facilities in the United States, by Profession, 2016 | |||||
|---|---|---|---|---|---|
| Profession | Total Staff Members | Total FTEsa | Percentage Certified in Addiction Treatment |
||
| Number | Percentage | Number | Percentage | ||
| Total (all types of professions) | 14,458 | 100 | 6,726 | 100 | 21 |
| Doctoral-level medical staff | 1,114 | 8 | 408 | 6 | 35 |
| Nursing staff or mid-level provider | 1,316 | 9 | 818 | 12 | 13 |
| Post-graduate level counselor | 2,228 | 15 | 1,134 | 17 | 25 |
| Bachelor's degree counselor | 1,349 | 9 | 659 | 10 | 33 |
| Associate's degree or no-degree counselor | 869 | 6 | 442 | 7 | 48 |
| Pharmacy assistant | 63 | <1 | 32 | <1 | 13 |
| Peer support staff | 1,026 | 7 | 337 | 5 | 18 |
| Care manager or patient navigator | 188 | 1 | 93 | 1 | 29 |
| Other recovery support worker | 759 | 5 | 238 | 4 | 14 |
| Administrative staff | 1,032 | 7 | 618 | 9 | 18 |
| Interns, contractors or per diem staff, and intake coordinators | 4,418 | 31 | 1,914 | 28 | 11 |
| Other clinical staff | 97 | 1 | 32 | <1 | 31 |
SOURCE: N-SSATS 2016, Question 23.
|
|||||
| TABLE B.9.a. Number and FTEs for Paid Medical Staff by Profession and State, 2016 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| State | Number of Staff | Number of FTEa | ||||||||||
| Total | Physician | Pharmacist | Registered Nurse | Licensed Practical Nurse |
Mid-Level Medical Personnel |
Total | Physician | Pharmacist | Registered Nurse | Licensed Practical Nurse |
Mid-Level Medical Personnel |
|
| Total | 55,665 | 14,811 | 2,016 | 22,238 | 10,316 | 6,284 | 37,318 | 7,576 | 1,110 | 16,515 | 8,073 | 4,043 |
| Alabama | 493 | 119 | 48 | 153 | 132 | 41 | 295 | 52 | 19 | 103 | 96 | 26 |
| Alaska | 146 | 61 | 4 | 35 | 21 | 25 | 98 | 32 | 4 | 28 | 16 | 18 |
| Arizona | 1,232 | 267 | 21 | 583 | 143 | 218 | 868 | 153 | 14 | 443 | 115 | 143 |
| Arkansas | 271 | 75 | 18 | 69 | 60 | 49 | 185 | 37 | 10 | 59 | 48 | 30 |
| California | 4,120 | 1,595 | 362 | 938 | 767 | 458 | 2,358 | 705 | 55 | 705 | 605 | 287 |
| Colorado | 655 | 208 | 24 | 211 | 71 | 141 | 398 | 113 | 22 | 140 | 41 | 83 |
| Connecticut | 1,129 | 302 | 39 | 379 | 213 | 196 | 654 | 150 | 13 | 244 | 140 | 108 |
| Delaware | 212 | 49 | 9 | 78 | 45 | 31 | 147 | 23 | 9 | 70 | 29 | 15 |
| District of Columbia | 112 | 38 | 5 | 33 | 15 | 21 | 63 | 18 | 3 | 17 | 10 | 15 |
| Florida | 3,680 | 972 | 135 | 1,170 | 965 | 438 | 2,797 | 653 | 77 | 961 | 799 | 308 |
| Georgia | 1,686 | 323 | 109 | 731 | 382 | 141 | 1,165 | 160 | 47 | 598 | 276 | 84 |
| Hawaii | 121 | 61 | 0 | 44 | 6 | 10 | 51 | 24 | 0 | 19 | 2 | 6 |
| Idaho | 198 | 38 | 11 | 63 | 32 | 54 | 102 | 15 | 3 | 42 | 18 | 24 |
| Illinois | 1,898 | 732 | 49 | 710 | 263 | 144 | 1,028 | 291 | 38 | 426 | 190 | 82 |
| Indiana | 1,224 | 251 | 24 | 622 | 199 | 128 | 889 | 169 | 17 | 472 | 148 | 82 |
| Iowa | 336 | 82 | 5 | 151 | 43 | 55 | 215 | 37 | 5 | 112 | 29 | 32 |
| Kansas | 582 | 130 | 20 | 200 | 133 | 99 | 475 | 87 | 13 | 180 | 120 | 75 |
| Kentucky | 840 | 195 | 19 | 415 | 109 | 102 | 511 | 92 | 15 | 300 | 54 | 50 |
| Louisiana | 742 | 213 | 24 | 208 | 255 | 42 | 476 | 100 | 15 | 148 | 192 | 21 |
| Maine | 488 | 113 | 21 | 264 | 26 | 64 | 295 | 57 | 8 | 167 | 20 | 44 |
| Maryland | 1,211 | 385 | 10 | 302 | 342 | 172 | 796 | 198 | 7 | 215 | 274 | 103 |
| Massachusetts | 1,953 | 516 | 34 | 818 | 355 | 230 | 1,278 | 251 | 20 | 629 | 238 | 140 |
| Michigan | 2,504 | 877 | 101 | 985 | 330 | 211 | 1,608 | 469 | 83 | 630 | 267 | 159 |
| Minnesota | 1,049 | 142 | 45 | 466 | 301 | 95 | 632 | 56 | 21 | 266 | 227 | 62 |
| Mississippi | 534 | 91 | 16 | 293 | 83 | 51 | 399 | 60 | 13 | 242 | 49 | 36 |
| Missouri | 933 | 210 | 14 | 443 | 209 | 57 | 752 | 127 | 12 | 406 | 166 | 41 |
| Montana | 580 | 113 | 51 | 291 | 76 | 49 | 517 | 106 | 40 | 257 | 72 | 42 |
| Nebraska | 375 | 108 | 32 | 117 | 41 | 77 | 240 | 71 | 24 | 79 | 34 | 33 |
| Nevada | 522 | 69 | 15 | 340 | 66 | 32 | 410 | 35 | 13 | 289 | 51 | 22 |
| New Hampshire | 331 | 144 | 6 | 51 | 40 | 90 | 258 | 104 | 1 | 47 | 34 | 72 |
| New Jersey | 1,360 | 423 | 30 | 586 | 189 | 132 | 772 | 184 | 12 | 400 | 112 | 64 |
| New Mexico | 492 | 158 | 41 | 162 | 57 | 74 | 309 | 70 | 18 | 124 | 42 | 54 |
| New York | 3,927 | 1,094 | 63 | 1,679 | 639 | 451 | 2,328 | 454 | 42 | 1,137 | 458 | 239 |
| North Carolina | 2,350 | 615 | 58 | 1,113 | 301 | 263 | 1,700 | 400 | 47 | 832 | 251 | 170 |
| North Dakota | 276 | 38 | 9 | 165 | 33 | 31 | 215 | 30 | 8 | 133 | 25 | 19 |
| Ohio | 2,109 | 593 | 57 | 812 | 433 | 214 | 1,413 | 284 | 38 | 627 | 333 | 131 |
| Oklahoma | 550 | 139 | 49 | 153 | 154 | 55 | 421 | 81 | 47 | 116 | 138 | 39 |
| Oregon | 517 | 140 | 25 | 153 | 114 | 85 | 350 | 65 | 23 | 113 | 101 | 48 |
| Pennsylvania | 2,904 | 729 | 79 | 1,088 | 804 | 204 | 2,039 | 304 | 67 | 824 | 718 | 126 |
| Puerto Rico | 615 | 219 | 13 | 317 | 57 | 9 | 409 | 111 | 12 | 237 | 42 | 8 |
| Rhode Island | 283 | 65 | 11 | 130 | 34 | 43 | 200 | 30 | 3 | 115 | 28 | 25 |
| South Carolina | 695 | 126 | 50 | 396 | 72 | 51 | 494 | 74 | 33 | 289 | 53 | 44 |
| South Dakota | 190 | 30 | 12 | 78 | 28 | 42 | 99 | 7 | 2 | 42 | 22 | 25 |
| Tennessee | 1,270 | 222 | 26 | 527 | 284 | 211 | 883 | 108 | 17 | 361 | 245 | 152 |
| Texas | 2,373 | 334 | 43 | 1,374 | 508 | 114 | 1,950 | 201 | 33 | 1,140 | 486 | 90 |
| Utah | 722 | 210 | 38 | 235 | 87 | 152 | 381 | 73 | 11 | 168 | 48 | 81 |
| Vermont | 224 | 61 | 10 | 80 | 38 | 35 | 150 | 42 | 3 | 60 | 21 | 25 |
| Virginia | 1,344 | 293 | 56 | 610 | 304 | 81 | 897 | 145 | 25 | 438 | 232 | 56 |
| Washington | 757 | 227 | 20 | 238 | 118 | 154 | 482 | 114 | 8 | 154 | 95 | 111 |
| West Virginia | 702 | 144 | 16 | 265 | 197 | 80 | 542 | 79 | 9 | 241 | 153 | 60 |
| Wisconsin | 1,541 | 438 | 35 | 858 | 110 | 100 | 1,072 | 257 | 28 | 641 | 84 | 63 |
| Wyoming | 101 | 27 | 2 | 48 | 4 | 20 | 52 | 13 | 1 | 28 | 2 | 8 |
| Other U.S. Territories | 207 | 7 | 2 | 8 | 28 | 162 | 203 | 5 | 2 | 6 | 28 | 162 |
SOURCE: N-SSATS 2016, Question 22.
|
||||||||||||
| TABLE B.9.b. Percentage of Medical Staff Certified in Addiction Treatment by Profession and State, 2016 | ||||||
|---|---|---|---|---|---|---|
| Total | Physician | Pharmacist | Registered Nurse | Licensed Practical Nurse |
Mid-Level Medical Personnel |
|
| Total | 19 | 42 | 23 | 8 | 10 | 20 |
| Alabama | 21 | 39 | 21 | 9 | 17 | 32 |
| Alaska | 17 | 28 | 0 | 9 | 14 | 8 |
| Arizona | 14 | 30 | 14 | 8 | 5 | 17 |
| Arkansas | 13 | 28 | 6 | 7 | 8 | 6 |
| California | 40 | 59 | 85 | 12 | 18 | 34 |
| Colorado | 19 | 39 | 0 | 9 | 3 | 14 |
| Connecticut | 24 | 47 | 28 | 8 | 18 | 26 |
| Delaware | 21 | 57 | 0 | 8 | 7 | 23 |
| District of Columbia | 39 | 45 | 40 | 36 | 60 | 19 |
| Florida | 21 | 36 | 22 | 12 | 16 | 26 |
| Georgia | 14 | 43 | 9 | 4 | 8 | 20 |
| Hawaii | 30 | 43 | NA | 11 | 0 | 40 |
| Idaho | 14 | 45 | 9 | 5 | 6 | 7 |
| Illinois | 27 | 48 | 8 | 13 | 16 | 14 |
| Indiana | 7 | 21 | 0 | 2 | 4 | 13 |
| Iowa | 7 | 18 | 0 | 1 | 5 | 11 |
| Kansas | 8 | 22 | 5 | 0 | 4 | 13 |
| Kentucky | 11 | 33 | 0 | 3 | 2 | 16 |
| Louisiana | 15 | 43 | 0 | 5 | 2 | 12 |
| Maine | 16 | 49 | 5 | 5 | 15 | 9 |
| Maryland | 26 | 50 | 10 | 13 | 11 | 27 |
| Massachusetts | 20 | 44 | 3 | 8 | 12 | 21 |
| Michigan | 12 | 23 | 1 | 7 | 7 | 9 |
| Minnesota | 17 | 45 | 16 | 10 | 11 | 25 |
| Mississippi | 6 | 26 | 0 | 1 | 1 | 12 |
| Missouri | 12 | 35 | 0 | 3 | 5 | 25 |
| Montana | 7 | 12 | 6 | 7 | 3 | 6 |
| Nebraska | 15 | 23 | 3 | 11 | 12 | 17 |
| Nevada | 16 | 42 | 0 | 9 | 9 | 9 |
| New Hampshire | 21 | 42 | 17 | 2 | 2 | 6 |
| New Jersey | 25 | 48 | 13 | 11 | 14 | 33 |
| New Mexico | 18 | 30 | 15 | 9 | 12 | 16 |
| New York | 26 | 57 | 10 | 15 | 9 | 20 |
| North Carolina | 15 | 37 | 5 | 4 | 5 | 21 |
| North Dakota | 5 | 5 | 0 | 1 | 0 | 39 |
| Ohio | 19 | 38 | 4 | 10 | 13 | 13 |
| Oklahoma | 11 | 29 | 2 | 4 | 5 | 7 |
| Oregon | 17 | 40 | 0 | 12 | 1 | 13 |
| Pennsylvania | 12 | 36 | 3 | 2 | 5 | 14 |
| Puerto Rico | 33 | 47 | 23 | 23 | 32 | 33 |
| Rhode Island | 27 | 54 | 27 | 15 | 15 | 30 |
| South Carolina | 9 | 33 | 6 | 1 | 14 | 8 |
| South Dakota | 5 | 13 | 0 | 3 | 4 | 5 |
| Tennessee | 13 | 44 | 8 | 2 | 9 | 11 |
| Texas | 12 | 48 | 7 | 4 | 9 | 20 |
| Utah | 36 | 57 | 8 | 19 | 25 | 45 |
| Vermont | 18 | 38 | 40 | 5 | 11 | 17 |
| Virginia | 11 | 30 | 7 | 6 | 2 | 15 |
| Washington | 32 | 55 | 35 | 13 | 13 | 43 |
| West Virginia | 9 | 35 | 0 | 2 | 1 | 9 |
| Wisconsin | 13 | 35 | 9 | 3 | 1 | 18 |
| Wyoming | 16 | 33 | 0 | 8 | 0 | 15 |
| Other U.S. Territories | 7 | 43 | 0 | 25 | 7 | 5 |
| SOURCE: N-SSATS 2016, Question 22. NOTE: The percentages of staff who are certified in addiction treatment are calculated by dividing the number of staff certified in addiction treatment by the total number of staff in facilities that reported information on staff certification. Nearly all (99.8%) of the reported staff worked in facilities that reported counts of certified staff. |
||||||
| TABLE B.10.a. Number of FTEs for Paid Counseling and Support Staff by Profession and State, 2016 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| State | Number of Staff | Number of FTEa Staff | ||||||||||
| Total | Counselors | Support Staff | Total | Counselors | Support Staff | |||||||
| Post-Graduate Level | Bachelor's Degree | Associate's Degree or No-Degree |
Non-Administrative | Administrative | Post-Graduate Level | Bachelor's Degree | Associate's Degree or No-Degree |
Non-Administrative | Administrative | |||
| Total | 200,784 | 60,163 | 26,447 | 18,132 | 54,988 | 41,054 | 160,241 | 47,210 | 22,038 | 14,527 | 41,008 | 35,457 |
| Alabama | 1,450 | 637 | 130 | 41 | 320 | 322 | 1,112 | 482 | 118 | 26 | 214 | 272 |
| Alaska | 1,083 | 284 | 143 | 133 | 299 | 224 | 1,035 | 278 | 135 | 121 | 279 | 223 |
| Arizona | 6,442 | 1,590 | 668 | 368 | 2,639 | 1,178 | 5,320 | 1,255 | 533 | 296 | 2,199 | 1,038 |
| Arkansas | 1,188 | 356 | 177 | 154 | 232 | 269 | 907 | 252 | 149 | 123 | 159 | 223 |
| California | 19,155 | 3,871 | 1,865 | 4,331 | 5,591 | 3,498 | 14,907 | 2,918 | 1,500 | 3,348 | 4,036 | 3,105 |
| Colorado | 3,935 | 1,435 | 643 | 337 | 754 | 766 | 3,042 | 1,140 | 508 | 238 | 526 | 629 |
| Connecticut | 3,576 | 1,363 | 383 | 221 | 976 | 633 | 2,820 | 1,093 | 318 | 175 | 676 | 558 |
| Delaware | 520 | 167 | 95 | 46 | 87 | 125 | 427 | 137 | 74 | 41 | 65 | 112 |
| District of Columbia | 400 | 128 | 53 | 42 | 99 | 78 | 298 | 91 | 44 | 37 | 67 | 60 |
| Florida | 12,359 | 3,215 | 1,238 | 648 | 5,096 | 2,163 | 9,938 | 2,560 | 1,027 | 524 | 3,896 | 1,932 |
| Georgia | 5,153 | 1,702 | 770 | 506 | 1,214 | 961 | 3,616 | 1,085 | 489 | 412 | 784 | 846 |
| Hawaii | 1,953 | 603 | 309 | 218 | 532 | 291 | 1,082 | 340 | 233 | 180 | 207 | 123 |
| Idaho | 1,438 | 587 | 173 | 84 | 305 | 289 | 976 | 376 | 121 | 61 | 168 | 250 |
| Illinois | 7,193 | 2,263 | 1,345 | 612 | 1,378 | 1,595 | 5,410 | 1,702 | 1,053 | 476 | 938 | 1,241 |
| Indiana | 4,853 | 1,590 | 1,079 | 335 | 893 | 956 | 4,157 | 1,335 | 972 | 285 | 709 | 855 |
| Iowa | 1,662 | 496 | 446 | 119 | 277 | 324 | 1,395 | 423 | 360 | 115 | 212 | 285 |
| Kansas | 2,366 | 748 | 255 | 129 | 711 | 523 | 2,019 | 646 | 218 | 123 | 564 | 468 |
| Kentucky | 4,482 | 1,322 | 628 | 389 | 1,275 | 868 | 3,248 | 1,011 | 401 | 73 | 1,043 | 720 |
| Louisiana | 1,694 | 466 | 176 | 91 | 573 | 388 | 1,386 | 373 | 138 | 74 | 466 | 334 |
| Maine | 1,608 | 510 | 222 | 109 | 430 | 338 | 1,244 | 372 | 182 | 98 | 315 | 278 |
| Maryland | 4,338 | 1,296 | 644 | 475 | 939 | 984 | 3,414 | 999 | 524 | 387 | 650 | 853 |
| Massachusetts | 6,239 | 2,314 | 634 | 459 | 1,679 | 1,153 | 4,807 | 1,778 | 535 | 329 | 1,197 | 968 |
| Michigan | 7,790 | 3,167 | 601 | 287 | 1,932 | 1,803 | 6,340 | 2,418 | 515 | 235 | 1,590 | 1,582 |
| Minnesota | 4,460 | 912 | 1,057 | 333 | 1,286 | 872 | 3,639 | 748 | 928 | 284 | 933 | 745 |
| Mississippi | 1,474 | 545 | 172 | 61 | 454 | 242 | 1,203 | 455 | 148 | 52 | 325 | 222 |
| Missouri | 4,269 | 908 | 366 | 206 | 1,966 | 822 | 3,421 | 760 | 303 | 163 | 1,438 | 758 |
| Montana | 979 | 151 | 118 | 59 | 350 | 301 | 870 | 137 | 110 | 46 | 317 | 259 |
| Nebraska | 1,515 | 551 | 124 | 51 | 459 | 330 | 1,232 | 420 | 111 | 47 | 355 | 298 |
| Nevada | 1,253 | 247 | 173 | 59 | 460 | 314 | 992 | 200 | 127 | 54 | 339 | 273 |
| New Hampshire | 1,633 | 662 | 156 | 58 | 275 | 482 | 1,435 | 558 | 153 | 52 | 205 | 467 |
| New Jersey | 4,383 | 1,531 | 580 | 384 | 956 | 932 | 3,418 | 1,153 | 491 | 350 | 638 | 787 |
| New Mexico | 1,993 | 720 | 135 | 111 | 464 | 563 | 1,630 | 555 | 113 | 83 | 372 | 506 |
| New York | 11,661 | 3,487 | 1,705 | 1,737 | 2,143 | 2,589 | 8,820 | 2,667 | 1,422 | 1,376 | 1,279 | 2,076 |
| North Carolina | 6,723 | 2,391 | 964 | 417 | 1,465 | 1,487 | 5,445 | 1,913 | 799 | 370 | 1,121 | 1,242 |
| North Dakota | 1,204 | 269 | 203 | 72 | 436 | 224 | 997 | 225 | 172 | 51 | 354 | 194 |
| Ohio | 8,738 | 2,601 | 1,269 | 807 | 2,170 | 1,891 | 7,276 | 2,237 | 1,135 | 686 | 1,562 | 1,656 |
| Oklahoma | 3,080 | 1,174 | 379 | 93 | 764 | 670 | 2,520 | 883 | 307 | 87 | 626 | 617 |
| Oregon | 3,212 | 932 | 539 | 434 | 615 | 693 | 2,730 | 767 | 487 | 396 | 466 | 614 |
| Pennsylvania | 7,585 | 2,470 | 1,286 | 246 | 1,950 | 1,634 | 6,136 | 1,973 | 1,109 | 199 | 1,457 | 1,398 |
| Puerto Rico | 1,210 | 257 | 124 | 32 | 447 | 350 | 893 | 194 | 96 | 22 | 317 | 263 |
| Rhode Island | 982 | 250 | 181 | 69 | 263 | 219 | 815 | 214 | 172 | 64 | 200 | 164 |
| South Carolina | 1,715 | 684 | 167 | 30 | 412 | 422 | 1,405 | 554 | 151 | 28 | 316 | 357 |
| South Dakota | 936 | 180 | 166 | 106 | 306 | 178 | 822 | 165 | 153 | 100 | 240 | 165 |
| Tennessee | 4,314 | 1,128 | 603 | 148 | 1,503 | 932 | 3,577 | 913 | 532 | 132 | 1,156 | 845 |
| Texas | 6,039 | 1,344 | 652 | 648 | 2,227 | 1,168 | 5,051 | 1,068 | 558 | 539 | 1,818 | 1,067 |
| Utah | 3,828 | 1,081 | 295 | 241 | 1,607 | 604 | 2,947 | 793 | 247 | 189 | 1,199 | 519 |
| Vermont | 888 | 366 | 117 | 82 | 159 | 164 | 724 | 309 | 101 | 71 | 103 | 141 |
| Virginia | 4,514 | 1,718 | 704 | 243 | 1,060 | 789 | 3,918 | 1,505 | 620 | 220 | 880 | 694 |
| Washington | 5,408 | 1,195 | 929 | 991 | 1,229 | 1,063 | 4,680 | 1,029 | 832 | 863 | 1,002 | 953 |
| West Virginia | 1,409 | 430 | 236 | 71 | 354 | 318 | 1,195 | 358 | 206 | 63 | 282 | 286 |
| Wisconsin | 3,683 | 1,571 | 324 | 183 | 706 | 899 | 2,857 | 1,138 | 269 | 142 | 519 | 790 |
| Wyoming | 683 | 279 | 33 | 16 | 208 | 147 | 571 | 240 | 27 | 13 | 171 | 120 |
| Other U.S. Territories | 138 | 21 | 15 | 10 | 64 | 28 | 123 | 15 | 15 | 9 | 57 | 27 |
SOURCE: N-SSATS 2016, Question 22.
|
||||||||||||
| TABLE B.10.b. Percentages of Counseling and Other Support Staff Certified in Addiction Treatment by Profession and State, 2016 | ||||||
|---|---|---|---|---|---|---|
| State | Total | Counselors | Support Staff | |||
| Post-Graduate Level | Bachelor's Degree | Associate's Degree or No-Degree |
Non-Administrative | Administrative | ||
| Total | 30 | 40 | 49 | 59 | 17 | 7 |
| Alabama | 39 | 53 | 62 | 44 | 29 | 10 |
| Alaska | 26 | 45 | 42 | 38 | 9 | 8 |
| Arizona | 13 | 30 | 15 | 17 | 7 | 2 |
| Arkansas | 24 | 24 | 40 | 45 | 18 | 5 |
| California | 44 | 39 | 65 | 76 | 34 | 14 |
| Colorado | 37 | 47 | 53 | 68 | 21 | 9 |
| Connecticut | 23 | 32 | 37 | 39 | 13 | 7 |
| Delaware | 32 | 43 | 68 | 37 | 15 | 2 |
| District of Columbia | 40 | 51 | 75 | 90 | 10 | 8 |
| Florida | 20 | 36 | 32 | 33 | 11 | 8 |
| Georgia | 20 | 25 | 32 | 24 | 17 | 3 |
| Hawaii | 33 | 66 | 20 | 34 | 18 | 5 |
| Idaho | 38 | 50 | 61 | 73 | 20 | 7 |
| Illinois | 41 | 49 | 53 | 68 | 36 | 15 |
| Indiana | 17 | 30 | 19 | 12 | 8 | 2 |
| Iowa | 34 | 43 | 59 | 30 | 15 | 2 |
| Kansas | 34 | 55 | 92 | 53 | 10 | 7 |
| Kentucky | 26 | 32 | 43 | 86 | 9 | 3 |
| Louisiana | 23 | 33 | 64 | 69 | 8 | 5 |
| Maine | 36 | 56 | 67 | 50 | 16 | 7 |
| Maryland | 45 | 56 | 84 | 71 | 25 | 10 |
| Massachusetts | 17 | 21 | 31 | 31 | 11 | 4 |
| Michigan | 29 | 45 | 42 | 51 | 19 | 4 |
| Minnesota | 43 | 53 | 87 | 67 | 16 | 10 |
| Mississippi | 11 | 17 | 10 | 20 | 8 | 2 |
| Missouri | 26 | 53 | 71 | 71 | 11 | 4 |
| Montana | 29 | 71 | 85 | 78 | 6 | 5 |
| Nebraska | 28 | 55 | 41 | 63 | 6 | 4 |
| Nevada | 32 | 63 | 64 | 80 | 15 | 7 |
| New Hampshire | 17 | 17 | 29 | 47 | 22 | 7 |
| New Jersey | 30 | 51 | 40 | 37 | 12 | 6 |
| New Mexico | 29 | 38 | 61 | 76 | 22 | 6 |
| New York | 38 | 42 | 65 | 60 | 29 | 9 |
| North Carolina | 32 | 51 | 41 | 44 | 19 | 5 |
| North Dakota | 19 | 32 | 59 | 8 | 3 | 0 |
| Ohio | 33 | 40 | 54 | 64 | 25 | 6 |
| Oklahoma | 30 | 50 | 34 | 29 | 19 | 4 |
| Oregon | 36 | 38 | 60 | 71 | 23 | 6 |
| Pennsylvania | 18 | 26 | 29 | 25 | 10 | 3 |
| Puerto Rico | 35 | 49 | 55 | 78 | 34 | 15 |
| Rhode Island | 26 | 45 | 39 | 49 | 12 | 5 |
| South Carolina | 32 | 52 | 60 | 60 | 13 | 4 |
| South Dakota | 36 | 66 | 66 | 60 | 12 | 6 |
| Tennessee | 14 | 16 | 11 | 29 | 13 | 12 |
| Texas | 33 | 38 | 75 | 79 | 16 | 9 |
| Utah | 21 | 41 | 41 | 27 | 9 | 6 |
| Vermont | 31 | 55 | 38 | 13 | 9 | 1 |
| Virginia | 15 | 22 | 18 | 38 | 7 | 2 |
| Washington | 45 | 45 | 69 | 74 | 30 | 13 |
| West Virginia | 10 | 22 | 6 | 13 | 7 | 1 |
| Wisconsin | 33 | 45 | 58 | 87 | 19 | 3 |
| Wyoming | 22 | 33 | 55 | 75 | 13 | 2 |
| Other U.S. Territories | 16 | 43 | 60 | 40 | 0 | 0 |
| SOURCE: N-SSATS 2016, Question 22. NOTE: The percentages of staff who are certified in addiction treatment are calculated by dividing the number of staff certified in addiction treatment by the total number of staff in facilities that reported information on staff certification. Nearly all (99.6%) of the reported staff worked in facilities that reported counts of certified staff. |
||||||
| TABLE B.11.a. FTE Medical Staff and Percentage Certified in Addiction Treatment by Profession and Facility Characteristic, 2016 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Facility Type | FTEa Staff | Percentage Certified in Addiction Treatment | ||||||||||
| Total | Physician | Pharmacist | Registered Nurse | Licensed Practical Nurse |
Mid-Level Medical Personnel |
Total | Physician | Pharmacist | Registered Nurse | Licensed Practical Nurse |
Mid-Level Medical Personnel |
|
| Total | 37,318 | 7,576 | 1,110 | 16,515 | 8,073 | 4,043 | 19 | 42 | 23 | 8 | 10 | 20 |
| Facility focus | ||||||||||||
| SUD treatment | 14,184 | 2,619 | 264 | 5,301 | 4,645 | 1,355 | 30 | 61 | 40 | 15 | 13 | 31 |
| MH treatment | 5,381 | 922 | 157 | 3,239 | 636 | 428 | 5 | 15 | 4 | 2 | 1 | 6 |
| SUD and MH treatment | 13,782 | 3,110 | 432 | 6,448 | 2,205 | 1,586 | 15 | 34 | 10 | 5 | 7 | 18 |
| Other | 3,971 | 926 | 258 | 1,527 | 586 | 674 | 4 | 11 | 2 | 1 | 2 | 5 |
| Operation | ||||||||||||
| Private NP | 15,569 | 3,315 | 361 | 6,888 | 2,986 | 2,019 | 21 | 40 | 42 | 9 | 13 | 19 |
| Private FP | 12,889 | 2,315 | 248 | 5,781 | 3,498 | 1,048 | 22 | 53 | 14 | 7 | 10 | 29 |
| Public | 8,860 | 1,946 | 501 | 3,846 | 1,589 | 977 | 10 | 25 | 3 | 5 | 3 | 8 |
| Federally certified OTP | ||||||||||||
| OTP | 6,502 | 1,023 | 167 | 2,116 | 2,625 | 571 | 26 | 61 | 17 | 14 | 14 | 31 |
| Not OTP | 30,815 | 6,552 | 943 | 14,399 | 5,448 | 3,473 | 18 | 38 | 24 | 6 | 8 | 18 |
| Any pharmacotherapy | ||||||||||||
| Provide | 30,509 | 5,661 | 951 | 13,922 | 6,980 | 2,994 | 19 | 45 | 24 | 8 | 10 | 19 |
| Do not provide | 6,809 | 1,915 | 159 | 2,593 | 1,093 | 1,049 | 20 | 33 | 6 | 8 | 10 | 23 |
| Any pharmacotherapy for opioid disorders | ||||||||||||
| Provide | 27,801 | 5,089 | 863 | 12,574 | 6,589 | 2,686 | 20 | 47 | 26 | 8 | 10 | 20 |
| Do not provide | 9,517 | 2,487 | 247 | 3,941 | 1,484 | 1,357 | 17 | 31 | 5 | 6 | 8 | 20 |
| SOURCE: N-SSATS 2016, Question 22. NOTE: The percentages of staff who are certified in addiction treatment are calculated by dividing the number of staff certified in addiction treatment by the total number of staff in facilities that reported information on staff certification. Nearly all (99.6%) of the reported staff worked in facilities that reported counts of certified staff. Facility operation was self-designated in N-SSATS Question 4 in 2013 and Question 7 in 2015.
|
||||||||||||
| TABLE B.11.b. FTE Counseling Staff and Percentage Certified in Addiction Treatment by Profession and Facility Characteristic, 2016 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Facility Type | FTEa Staff | Percentage Certified in Addiction Treatment | ||||||||||
| Total | Counselor | Support Staff | Total | Counselor | Staff Staff | |||||||
| Post-Graduate Level | Bachelor's Degree | Associate's Degree or No-Degree |
Non-Administrative Staff | Administrative Staff | Post-Graduate Level | Bachelor's Degree | Associate's Degree or No-Degree |
Non-Administrative Staff | Administrative Staff | |||
| Total | 160,241 | 47,210 | 22,038 | 14,527 | 41,008 | 35,457 | 30 | 40 | 49 | 59 | 17 | 7 |
| Facility focus | ||||||||||||
| SUD treatment | 73,862 | 17,537 | 11,709 | 9,591 | 19,796 | 15,229 | 41 | 58 | 64 | 67 | 24 | 11 |
| MH treatment | 18,518 | 6,503 | 2,401 | 785 | 4,786 | 4,044 | 9 | 16 | 10 | 14 | 4 | 2 |
| SUD and MH treatment | 62,660 | 21,805 | 7,550 | 3,858 | 14,897 | 14,550 | 24 | 33 | 37 | 49 | 14 | 5 |
| Other | 5,201 | 1,365 | 377 | 294 | 1,529 | 1,635 | 15 | 25 | 42 | 46 | 7 | 2 |
| Operation | ||||||||||||
| Private NP | 89,819 | 26,580 | 12,901 | 8,575 | 22,499 | 19,264 | 29 | 39 | 46 | 56 | 17 | 7 |
| Private FP | 47,773 | 13,340 | 6,598 | 4,128 | 12,630 | 11,078 | 33 | 43 | 52 | 62 | 21 | 8 |
| Public | 22,649 | 7,291 | 2,539 | 1,824 | 5,879 | 5,116 | 25 | 34 | 51 | 65 | 9 | 4 |
| Federally certified OTP | ||||||||||||
| OTP | 16,303 | 4,676 | 3,612 | 2,142 | 2,379 | 3,494 | 39 | 50 | 55 | 62 | 21 | 7 |
| Not OTP | 143,935 | 42,533 | 18,426 | 12,385 | 38,629 | 31,963 | 29 | 39 | 48 | 58 | 17 | 7 |
| Any pharmacotherapy | ||||||||||||
| Provide | 92,710 | 27,152 | 12,481 | 7,759 | 24,264 | 21,055 | 28 | 39 | 48 | 56 | 16 | 6 |
| Do not provide | 67,530 | 20,059 | 9,557 | 6,768 | 16,744 | 14,403 | 32 | 41 | 50 | 62 | 20 | 8 |
| Any pharmacotherapy for opioid disorders | ||||||||||||
| Provide | 81,070 | 23,334 | 11,249 | 6,884 | 21,245 | 18,359 | 29 | 40 | 48 | 57 | 17 | 6 |
| Do not provide | 79,171 | 23,877 | 10,789 | 7,643 | 19,763 | 17,099 | 31 | 39 | 49 | 60 | 18 | 8 |
| SOURCE: N-SSATS 2016, Question 22. NOTE: The percentages of staff who are certified in addiction treatment are calculated by dividing the number of staff certified in addiction treatment by the total number of staff in facilities that reported information on staff certification. Nearly all (99.6%) of the reported staff worked in facilities that reported counts of certified staff. Facility operation was self-designated in N-SSATS Question 7.
|
||||||||||||
| TABLE B.12.a. Number of Staff Hours per 100 Outpatient Clients per Week in Specialty SUD Treatment Facilities Providing Only Outpatient Services by Type of Staff and State, 2016 (all facilities) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| State | Total | Medical Staff | Counselor | Support Staff | ||||||
| Physician | Pharmacist | Mid-Level Medical Personnel |
Registered Nurse | Licensed Practical Nurse |
Post-Graduate Level | Bachelor's Degree | Associate's Degree or No-Degree |
|||
| Total | 292 | 15 | 3 | 9 | 14 | 13 | 113 | 51 | 27 | 47 |
| Alabama | 238 | 11 | 8 | 4 | 15 | 21 | 123 | 26 | 3 | 27 |
| Alaska | 537 | 32 | 15 | 16 | 9 | 8 | 213 | 66 | 74 | 104 |
| Arizona | 300 | 9 | 1 | 11 | 8 | 10 | 86 | 42 | 18 | 113 |
| Arkansas | 295 | 14 | 5 | 12 | 5 | 27 | 136 | 45 | 21 | 31 |
| California | 289 | 19 | 1 | 8 | 7 | 11 | 78 | 41 | 73 | 51 |
| Colorado | 237 | 9 | 3 | 10 | 8 | 3 | 110 | 39 | 16 | 38 |
| Connecticut | 197 | 10 | 0 | 9 | 8 | 12 | 86 | 26 | 8 | 39 |
| Delaware | 184 | 9 | 13 | 4 | 10 | 15 | 72 | 34 | 10 | 18 |
| District of Columbia | 329 | 26 | 4 | 22 | 22 | 10 | 110 | 48 | 54 | 32 |
| Florida | 368 | 29 | 3 | 8 | 12 | 22 | 131 | 54 | 13 | 95 |
| Georgia | 312 | 14 | 8 | 5 | 13 | 30 | 128 | 49 | 23 | 42 |
| Hawaii | 749 | 11 | 0 | 1 | 4 | 2 | 303 | 228 | 152 | 47 |
| Idaho | 384 | 3 | 0 | 13 | 4 | 5 | 193 | 67 | 34 | 65 |
| Illinois | 325 | 24 | 2 | 5 | 13 | 12 | 133 | 66 | 30 | 41 |
| Indiana | 384 | 11 | 2 | 7 | 15 | 12 | 129 | 133 | 39 | 37 |
| Iowa | 455 | 11 | 2 | 14 | 22 | 7 | 175 | 156 | 22 | 46 |
| Kansas | 550 | 20 | 8 | 25 | 34 | 20 | 200 | 64 | 40 | 140 |
| Kentucky | 247 | 10 | 0 | 6 | 4 | 5 | 112 | 43 | 6 | 61 |
| Louisiana | 258 | 20 | 7 | 3 | 12 | 21 | 102 | 34 | 19 | 40 |
| Maine | 284 | 11 | 4 | 6 | 22 | 7 | 107 | 49 | 18 | 60 |
| Maryland | 201 | 12 | 1 | 6 | 10 | 17 | 66 | 36 | 25 | 26 |
| Massachusetts | 187 | 9 | 1 | 8 | 11 | 7 | 112 | 12 | 3 | 25 |
| Michigan | 261 | 15 | 2 | 5 | 9 | 10 | 140 | 24 | 9 | 47 |
| Minnesota | 437 | 7 | 8 | 9 | 38 | 19 | 116 | 143 | 35 | 62 |
| Mississippi | 964 | 59 | 12 | 23 | 82 | 18 | 472 | 144 | 16 | 138 |
| Missouri | 275 | 13 | 0 | 6 | 12 | 11 | 84 | 46 | 23 | 80 |
| Montana | 473 | 40 | 18 | 24 | 57 | 48 | 99 | 77 | 43 | 68 |
| Nebraska | 524 | 53 | 18 | 25 | 20 | 15 | 251 | 47 | 26 | 70 |
| Nevada | 249 | 15 | 11 | 6 | 15 | 14 | 65 | 45 | 22 | 56 |
| New Hampshire | 107 | 8 | 0 | 6 | 5 | 14 | 35 | 20 | 7 | 11 |
| New Jersey | 300 | 17 | 2 | 5 | 20 | 8 | 131 | 54 | 34 | 29 |
| New Mexico | 260 | 13 | 9 | 12 | 17 | 8 | 106 | 24 | 19 | 52 |
| New York | 192 | 10 | 0 | 5 | 16 | 6 | 79 | 35 | 24 | 17 |
| North Carolina | 366 | 34 | 4 | 10 | 26 | 17 | 150 | 57 | 24 | 43 |
| North Dakota | 958 | 52 | 15 | 42 | 111 | 3 | 328 | 85 | 12 | 309 |
| Ohio | 442 | 18 | 5 | 10 | 24 | 17 | 172 | 78 | 33 | 85 |
| Oklahoma | 325 | 12 | 13 | 7 | 15 | 18 | 145 | 52 | 8 | 55 |
| Oregon | 327 | 10 | 7 | 8 | 11 | 15 | 125 | 62 | 54 | 36 |
| Pennsylvania | 223 | 10 | 1 | 3 | 6 | 15 | 101 | 54 | 6 | 26 |
| Puerto Rico | 167 | 22 | 1 | 3 | 32 | 7 | 47 | 30 | 2 | 23 |
| Rhode Island | 264 | 9 | 1 | 11 | 29 | 10 | 76 | 49 | 16 | 63 |
| South Carolina | 147 | 6 | 5 | 2 | 4 | 5 | 80 | 31 | 5 | 10 |
| South Dakota | 523 | 6 | 4 | 20 | 19 | 14 | 170 | 149 | 75 | 65 |
| Tennessee | 421 | 18 | 10 | 29 | 24 | 30 | 136 | 76 | 8 | 90 |
| Texas | 240 | 13 | 1 | 8 | 7 | 17 | 57 | 52 | 47 | 38 |
| Utah | 269 | 8 | 1 | 14 | 9 | 7 | 128 | 41 | 17 | 45 |
| Vermont | 376 | 18 | 0 | 10 | 13 | 13 | 210 | 72 | 13 | 28 |
| Virginia | 548 | 19 | 4 | 7 | 21 | 28 | 230 | 93 | 21 | 125 |
| Washington | 319 | 6 | 0 | 11 | 8 | 6 | 100 | 76 | 75 | 37 |
| West Virginia | 212 | 11 | 0 | 9 | 8 | 19 | 71 | 54 | 3 | 35 |
| Wisconsin | 330 | 22 | 4 | 9 | 22 | 8 | 173 | 36 | 19 | 37 |
| Wyoming | 350 | 7 | 2 | 7 | 12 | 2 | 192 | 30 | 13 | 85 |
| SOURCE: N-SSATS 2016, Question 22. | ||||||||||
| TABLE B.12.b. Number of Staff Hours per 100 Outpatient Clients per Week in Specialty SUD Treatment Facilities Providing Only Outpatient Services by Type of Staff and State, 2016 (facilities providing any pharmacotherapy) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| State | Total | Medical Staff | Counselor | Support Staff | ||||||
| Physician | Pharmacist | Mid-Level Medical Personnel |
Registered Nurse | Licensed Practical Nurse |
Post-Graduate Level | Bachelor's Degree | Associate's Degree or No-Degree |
|||
| Total | 242 | 15 | 3 | 9 | 15 | 17 | 87 | 39 | 20 | 36 |
| Alabama | 194 | 10 | 10 | 3 | 15 | 25 | 94 | 24 | 2 | 12 |
| Alaska | 412 | 28 | 26 | 28 | 11 | 15 | 142 | 26 | 16 | 118 |
| Arizona | 204 | 10 | 1 | 12 | 10 | 15 | 47 | 23 | 12 | 74 |
| Arkansas | 246 | 17 | 10 | 5 | 6 | 46 | 61 | 47 | 17 | 36 |
| California | 237 | 21 | 1 | 9 | 9 | 17 | 66 | 31 | 50 | 34 |
| Colorado | 268 | 11 | 5 | 13 | 12 | 5 | 123 | 41 | 18 | 40 |
| Connecticut | 162 | 9 | 0 | 9 | 8 | 13 | 69 | 15 | 7 | 31 |
| Delaware | 176 | 9 | 15 | 4 | 10 | 16 | 63 | 31 | 11 | 18 |
| District of Columbia | 219 | 24 | 5 | 20 | 20 | 13 | 37 | 30 | 50 | 20 |
| Florida | 308 | 25 | 4 | 9 | 14 | 33 | 83 | 37 | 13 | 89 |
| Georgia | 227 | 13 | 10 | 4 | 9 | 34 | 77 | 40 | 19 | 20 |
| Hawaii | 190 | 9 | 0 | 1 | 9 | 4 | 71 | 14 | 45 | 35 |
| Idaho | 457 | 7 | 0 | 38 | 5 | 11 | 257 | 53 | 24 | 62 |
| Illinois | 291 | 22 | 2 | 6 | 16 | 16 | 117 | 60 | 22 | 30 |
| Indiana | 342 | 9 | 0 | 7 | 15 | 17 | 99 | 134 | 41 | 21 |
| Iowa | 372 | 8 | 7 | 17 | 28 | 11 | 162 | 84 | 11 | 45 |
| Kansas | 736 | 35 | 15 | 39 | 57 | 31 | 245 | 42 | 55 | 216 |
| Kentucky | 194 | 10 | 0 | 6 | 8 | 10 | 94 | 37 | 5 | 24 |
| Louisiana | 212 | 17 | 8 | 4 | 13 | 26 | 83 | 22 | 10 | 30 |
| Maine | 207 | 17 | 6 | 9 | 27 | 10 | 52 | 40 | 23 | 22 |
| Maryland | 180 | 13 | 1 | 6 | 11 | 20 | 56 | 33 | 22 | 17 |
| Massachusetts | 162 | 10 | 1 | 7 | 14 | 9 | 90 | 9 | 3 | 19 |
| Michigan | 273 | 22 | 3 | 6 | 13 | 17 | 141 | 20 | 9 | 42 |
| Minnesota | 297 | 7 | 5 | 4 | 14 | 26 | 85 | 91 | 23 | 42 |
| Mississippi | 1126 | 188 | 41 | 34 | 167 | 69 | 464 | 54 | 28 | 83 |
| Missouri | 219 | 16 | 0 | 9 | 12 | 14 | 73 | 33 | 13 | 49 |
| Montana | 394 | 61 | 5 | 12 | 82 | 65 | 76 | 55 | 29 | 8 |
| Nebraska | 513 | 40 | 28 | 37 | 30 | 25 | 207 | 31 | 32 | 84 |
| Nevada | 241 | 20 | 13 | 7 | 21 | 19 | 46 | 34 | 18 | 63 |
| New Hampshire | 90 | 8 | 0 | 3 | 4 | 15 | 25 | 17 | 8 | 10 |
| New Jersey | 251 | 14 | 2 | 4 | 23 | 9 | 99 | 47 | 30 | 22 |
| New Mexico | 234 | 16 | 13 | 14 | 23 | 11 | 75 | 25 | 19 | 39 |
| New York | 185 | 10 | 0 | 6 | 17 | 6 | 75 | 35 | 20 | 15 |
| North Carolina | 264 | 31 | 5 | 8 | 28 | 21 | 101 | 28 | 14 | 28 |
| North Dakota | 1114 | 76 | 25 | 6 | 163 | 5 | 346 | 20 | 0 | 472 |
| Ohio | 404 | 20 | 6 | 10 | 29 | 22 | 127 | 71 | 27 | 94 |
| Oklahoma | 151 | 11 | 12 | 5 | 11 | 17 | 51 | 23 | 3 | 18 |
| Oregon | 307 | 12 | 11 | 11 | 16 | 27 | 80 | 60 | 52 | 37 |
| Pennsylvania | 221 | 11 | 1 | 4 | 6 | 21 | 96 | 51 | 6 | 25 |
| Puerto Rico | 151 | 22 | 1 | 2 | 32 | 8 | 39 | 26 | 0 | 21 |
| Rhode Island | 279 | 10 | 1 | 12 | 31 | 11 | 75 | 50 | 18 | 70 |
| South Carolina | 133 | 10 | 11 | 0 | 5 | 12 | 44 | 39 | 8 | 4 |
| South Dakota | 481 | 8 | 0 | 22 | 16 | 22 | 132 | 137 | 73 | 71 |
| Tennessee | 247 | 12 | 5 | 15 | 8 | 27 | 77 | 38 | 2 | 62 |
| Texas | 201 | 16 | 1 | 8 | 8 | 28 | 36 | 41 | 35 | 28 |
| Utah | 222 | 10 | 1 | 18 | 11 | 9 | 88 | 34 | 14 | 38 |
| Vermont | 373 | 19 | 0 | 13 | 17 | 16 | 204 | 62 | 15 | 26 |
| Virginia | 398 | 17 | 4 | 6 | 17 | 31 | 177 | 57 | 18 | 71 |
| Washington | 204 | 7 | 1 | 9 | 14 | 14 | 44 | 48 | 44 | 23 |
| West Virginia | 157 | 11 | 0 | 9 | 7 | 21 | 49 | 45 | 0 | 14 |
| Wisconsin | 362 | 26 | 6 | 10 | 28 | 12 | 174 | 48 | 20 | 39 |
| Wyoming | 388 | 15 | 4 | 9 | 19 | 4 | 210 | 35 | 11 | 80 |
| SOURCE: N-SSATS 2016, Question 22. | ||||||||||
| TABLE B.12.c. Number of Staff Hours per 100 Outpatient Clients per Week in Specialty SUD Treatment Facilities Providing Only Outpatient Services by Type of Staff and State, 2016 (facilities providing no pharmacotherapy) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| State | Total | Medical Staff | Counselor | Support Staff | ||||||
| Physician | Pharmacist | Mid-Level Medical Personnel |
Registered Nurse | Licensed Practical Nurse |
Post-Graduate Level | Bachelor's Degree | Associate's Degree or No-Degree |
|||
| Total | 393 | 14 | 2 | 8 | 10 | 4 | 167 | 75 | 42 | 72 |
| Alabama | 370 | 12 | 5 | 8 | 15 | 10 | 210 | 31 | 8 | 71 |
| Alaska | 668 | 36 | 3 | 3 | 7 | 0 | 287 | 107 | 133 | 90 |
| Arizona | 474 | 7 | 0 | 11 | 6 | 2 | 156 | 77 | 29 | 185 |
| Arkansas | 314 | 12 | 3 | 15 | 5 | 19 | 165 | 44 | 22 | 30 |
| California | 373 | 14 | 2 | 6 | 4 | 2 | 97 | 56 | 112 | 80 |
| Colorado | 186 | 5 | 0 | 5 | 2 | 0 | 89 | 37 | 15 | 33 |
| Connecticut | 490 | 13 | 0 | 8 | 4 | 0 | 227 | 116 | 16 | 106 |
| Delaware | 250 | 5 | 0 | 4 | 7 | 0 | 145 | 66 | 2 | 21 |
| District of Columbia | 720 | 35 | 0 | 31 | 28 | 0 | 370 | 111 | 69 | 76 |
| Florida | 459 | 36 | 1 | 6 | 10 | 6 | 204 | 80 | 13 | 103 |
| Georgia | 608 | 18 | 1 | 9 | 26 | 12 | 304 | 82 | 38 | 118 |
| Hawaii | 1261 | 12 | 0 | 1 | 0 | 0 | 516 | 424 | 250 | 58 |
| Idaho | 364 | 1 | 0 | 6 | 3 | 3 | 176 | 70 | 37 | 66 |
| Illinois | 374 | 28 | 1 | 3 | 8 | 6 | 156 | 75 | 42 | 56 |
| Indiana | 464 | 14 | 6 | 7 | 14 | 3 | 187 | 132 | 33 | 68 |
| Iowa | 497 | 12 | 0 | 12 | 20 | 4 | 182 | 192 | 27 | 47 |
| Kansas | 361 | 5 | 0 | 10 | 11 | 9 | 153 | 86 | 25 | 63 |
| Kentucky | 288 | 10 | 0 | 5 | 1 | 0 | 126 | 48 | 7 | 90 |
| Louisiana | 385 | 29 | 4 | 1 | 7 | 9 | 154 | 66 | 45 | 69 |
| Maine | 399 | 3 | 0 | 1 | 13 | 3 | 190 | 62 | 10 | 118 |
| Maryland | 318 | 11 | 1 | 4 | 4 | 2 | 124 | 54 | 42 | 76 |
| Massachusetts | 274 | 6 | 0 | 9 | 1 | 0 | 189 | 21 | 3 | 44 |
| Michigan | 249 | 8 | 0 | 3 | 5 | 3 | 139 | 28 | 10 | 52 |
| Minnesota | 603 | 6 | 12 | 15 | 67 | 10 | 152 | 205 | 48 | 87 |
| Mississippi | 916 | 21 | 3 | 20 | 57 | 3 | 474 | 170 | 13 | 155 |
| Missouri | 364 | 8 | 0 | 2 | 12 | 7 | 101 | 66 | 40 | 128 |
| Montana | 548 | 19 | 30 | 35 | 34 | 31 | 120 | 97 | 55 | 125 |
| Nebraska | 531 | 63 | 10 | 16 | 13 | 7 | 283 | 58 | 21 | 59 |
| Nevada | 267 | 6 | 7 | 4 | 3 | 3 | 103 | 69 | 30 | 42 |
| New Hampshire | 319 | 12 | 0 | 48 | 10 | 6 | 166 | 54 | 0 | 23 |
| New Jersey | 486 | 28 | 0 | 12 | 10 | 4 | 249 | 82 | 46 | 55 |
| New Mexico | 306 | 8 | 2 | 8 | 6 | 3 | 161 | 23 | 20 | 76 |
| New York | 241 | 11 | 0 | 3 | 10 | 0 | 106 | 36 | 45 | 30 |
| North Carolina | 764 | 44 | 2 | 19 | 19 | 4 | 339 | 172 | 64 | 102 |
| North Dakota | 731 | 18 | 0 | 94 | 37 | 0 | 302 | 179 | 30 | 71 |
| Ohio | 519 | 15 | 2 | 9 | 12 | 6 | 266 | 94 | 46 | 68 |
| Oklahoma | 572 | 14 | 15 | 11 | 20 | 21 | 276 | 94 | 16 | 106 |
| Oregon | 345 | 8 | 4 | 5 | 7 | 4 | 167 | 64 | 55 | 34 |
| Pennsylvania | 228 | 9 | 0 | 1 | 4 | 1 | 114 | 62 | 6 | 30 |
| Puerto Rico | 327 | 22 | 0 | 10 | 37 | 0 | 130 | 67 | 21 | 42 |
| Rhode Island | 149 | 5 | 0 | 6 | 8 | 0 | 80 | 41 | 0 | 8 |
| South Carolina | 158 | 3 | 0 | 3 | 3 | 0 | 107 | 26 | 2 | 14 |
| South Dakota | 564 | 5 | 7 | 18 | 21 | 7 | 207 | 161 | 78 | 60 |
| Tennessee | 750 | 31 | 18 | 54 | 54 | 37 | 247 | 147 | 20 | 141 |
| Texas | 296 | 9 | 1 | 8 | 6 | 1 | 86 | 67 | 64 | 53 |
| Utah | 394 | 5 | 0 | 5 | 2 | 1 | 235 | 61 | 24 | 63 |
| Vermont | 386 | 15 | 0 | 0 | 0 | 0 | 229 | 104 | 4 | 34 |
| Virginia | 991 | 24 | 4 | 11 | 33 | 22 | 385 | 198 | 30 | 285 |
| Washington | 404 | 6 | 0 | 12 | 3 | 1 | 140 | 96 | 98 | 48 |
| West Virginia | 464 | 11 | 0 | 10 | 14 | 13 | 172 | 96 | 19 | 128 |
| Wisconsin | 277 | 15 | 1 | 6 | 14 | 3 | 172 | 16 | 16 | 34 |
| Wyoming | 320 | 0 | 0 | 6 | 7 | 0 | 178 | 27 | 15 | 88 |
| SOURCE: N-SSATS 2016, Question 22. | ||||||||||
| TABLE B.13. Number of Staff Hours per 100 Outpatient Clients per Week in Specialty SUD Treatment Facilities Providing Only Outpatient Services, by Type of Services Offered at Facility, 2016 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Type of Facility | Total | Medical Staff | Counselor | Support Staff | ||||||
| Physician | Pharmacist | Mid-Level Medical Personnel |
Registered Nurse | Licensed Practical Nurse |
Post-Graduate Level | Bachelor's Degree | Associate's Degree or No-Degree |
|||
| Total | 292 | 15 | 3 | 9 | 14 | 13 | 113 | 51 | 27 | 47 |
| Federally certified OTP | ||||||||||
| OTP | 135 | 7 | 2 | 4 | 10 | 21 | 35 | 31 | 17 | 8 |
| Not OTP | 397 | 20 | 4 | 11 | 16 | 7 | 166 | 64 | 34 | 74 |
| MH services | ||||||||||
| MH treatment offered | 322 | 17 | 3 | 10 | 15 | 12 | 131 | 53 | 26 | 55 |
| Screening only | 180 | 8 | 1 | 5 | 12 | 14 | 48 | 42 | 32 | 19 |
| No MH services | 154 | 5 | 1 | 3 | 5 | 16 | 35 | 42 | 31 | 14 |
| Screening for conditions other than SUDs | ||||||||||
| Yes | 293 | 25 | 9 | 18 | 30 | 25 | 81 | 39 | 24 | 42 |
| No | 291 | 12 | 1 | 6 | 10 | 10 | 121 | 54 | 28 | 49 |
| Outreach to people who may need treatment | ||||||||||
| Yes | 316 | 16 | 3 | 9 | 14 | 13 | 118 | 56 | 30 | 56 |
| No | 248 | 13 | 2 | 7 | 13 | 12 | 105 | 42 | 23 | 32 |
| Recovery support services | ||||||||||
| Yes | 373 | 17 | 4 | 10 | 17 | 16 | 132 | 68 | 34 | 76 |
| No | 269 | 14 | 3 | 8 | 13 | 12 | 108 | 46 | 25 | 40 |
| Facility focus | ||||||||||
| SUD treatment | 193 | 9 | 1 | 4 | 9 | 13 | 63 | 41 | 28 | 25 |
| MH treatment | 1000 | 37 | 5 | 23 | 45 | 13 | 443 | 201 | 35 | 198 |
| SUD and MH treatment | 405 | 21 | 4 | 11 | 15 | 8 | 187 | 57 | 25 | 77 |
| Other | 905 | 101 | 53 | 120 | 133 | 75 | 187 | 48 | 33 | 157 |
| SOURCE: N-SSATS 2016, Question 22. NOTE: Facilities were classified as a federally certified OTP if they indicated in Question 11 that they administer or dispense methadone, buprenorphine, or naltrexone (Vivitrol®) as a federally certified OTP. Facilities were classified as offering MH treatment if they said in response to Question 1a that they provided mental health services to substance abuse treatment clients (MHTXSA). Remaining facilities were classified as only screening if in Question 10 they indicated that they provided screening for mental health disorders (SRVC90) or provided comprehensive mental health assessment or diagnosis (SRVC2). Facilities not classified as offering MH treatment or screening only were classified as having no MH services. Facilities were identified as providing screening services for conditions other than SUDs if they indicated that they provide screening for hepatitis B, hepatitis C, HIV, sexually transmitted diseases, and tuberculosis (SRVC73 = 1, SRVC74 = 1, SRVC14 = 1, SRVC15 = 1, and SRVC16 = 1). Facilities were identified as providing recovery support services if they provide social skills development, mentoring or peer support, assistance obtaining social services, employment counseling or training, or assistance locating housing (SRVC96 = 1, SRVC97 = 1, SRVC36 = 1, SRVC39 = 1, and SRVC38 = 1). Facility focus was determined based on responses to Question 6. |
||||||||||
| TABLE B.14. Number of Staff Hours 100 Outpatient Clients per Week in Specialty SUD Treatment Facilities Providing Only Outpatient Services, by Facility Characteristics, 2016 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Type of Facility | Total | Medical Staff | Counselor | Support Staff | ||||||
| Physician | Pharmacist | Mid-Level Medical Personnel |
Registered Nurse | Licensed Practical Nurse |
Post-Graduate Level | Bachelor's Degree | Associate's Degree or No-Degree |
|||
| Total | 292 | 15 | 3 | 9 | 14 | 13 | 113 | 51 | 27 | 47 |
| Urbanicity | ||||||||||
| Urban | 278 | 15 | 3 | 7 | 13 | 13 | 110 | 48 | 26 | 44 |
| Rural | 370 | 14 | 4 | 11 | 17 | 13 | 138 | 69 | 34 | 69 |
| Operation | ||||||||||
| Private NP | 339 | 15 | 2 | 10 | 16 | 10 | 140 | 59 | 29 | 58 |
| Private FP | 206 | 11 | 2 | 5 | 6 | 15 | 74 | 41 | 23 | 29 |
| Public | 432 | 30 | 11 | 19 | 33 | 17 | 156 | 58 | 33 | 74 |
| Located in or operated by a hospital | ||||||||||
| Yes | 291 | 14 | 3 | 8 | 12 | 13 | 113 | 52 | 28 | 49 |
| No | 298 | 29 | 5 | 20 | 35 | 13 | 117 | 34 | 17 | 27 |
| Facility size | ||||||||||
| Small | 1606 | 81 | 17 | 46 | 74 | 28 | 671 | 257 | 137 | 294 |
| Medium | 506 | 27 | 5 | 16 | 20 | 11 | 205 | 81 | 44 | 97 |
| Large | 171 | 8 | 2 | 5 | 9 | 13 | 62 | 33 | 18 | 21 |
| Type of insurance accepted | ||||||||||
| Medicaid | 294 | 14 | 2 | 8 | 14 | 12 | 119 | 52 | 25 | 47 |
| Private insurance | 316 | 17 | 3 | 9 | 15 | 11 | 131 | 51 | 26 | 53 |
| SOURCE: N-SSATS 2016, Question 22. NOTE: Urbanicity is assigned based on the National Center for Health Statistics urbanicity classification scheme. Facilities in rural areas include those in micropolitan areas with an urban core population of at least 10,000 but less than 50,000, as well as those in non-core areas. Facilities in a central or fringe urban core with a population of 50,000 or more are considered urban. Information on urbanicity was not available for all facilities; urban and rural estimates are only reported for facilities with known urbanicity. Facility size was based on the number of outpatient clients in care. Facilities below the 25th percentile and above the 75th percentile for client count were identified as small and large, respectively. Remaining facilities were designated as medium size. Facility operation was self-designated in N-SSATS Question 7. |
||||||||||
| TABLE B.15. Number and Percentage of Facilities Providing Any Pharmacotherapy or Opioid-Related Pharmacotherapy, by Facility Characteristics, 2013 and 2016 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of Facilities | Percentage of Facilities | |||||||||||
| Providing Pharmacotherapies for Opioid Disorders |
Providing Any Pharmacotherapies |
Providing Pharmacotherapies for Opioid Disorders |
Providing Any Pharmacotherapies |
|||||||||
| 2013 | 2016 | Change | 2013 | 2016 | Change | 2013 | 2016 | Change | 2013 | 2016 | Change | |
| Total | 4,246 | 5,373 | 27 | 5,267 | 6,191 | 18 | 30 | 37 | 24 | 37 | 43 | 15 |
| Urbanicity | ||||||||||||
| Urban | 3,272 | 4,519 | 38 | 3,936 | 5,115 | 30 | 33 | 41 | 24 | 40 | 46 | 16 |
| Rural | 933 | 814 | -13 | 1,283 | 1,032 | -20 | 23 | 26 | 12 | 32 | 33 | 3 |
| Facility focus | ||||||||||||
| SUD treatment | NA | 3,253 | NA | NA | 3,519 | NA | NA | 41 | NA | NA | 44 | NA |
| MH treatment | NA | 242 | NA | NA | 347 | NA | NA | 24 | NA | NA | 35 | NA |
| SUD and MH treatment | NA | 1,707 | NA | NA | 2,126 | NA | NA | 34 | NA | NA | 42 | NA |
| Other | NA | 171 | NA | NA | 199 | NA | NA | 43 | NA | NA | 50 | NA |
| Operation | ||||||||||||
| Private, NP | 2,101 | 2,644 | 26 | 2,622 | 3,071 | 17 | 27 | 35 | 28 | 34 | 40 | 20 |
| Private, FP | 1,582 | 2,101 | 33 | 1,838 | 2,296 | 25 | 35 | 41 | 19 | 40 | 45 | 12 |
| Public | 563 | 628 | 12 | 807 | 824 | 2 | 32 | 38 | 20 | 46 | 50 | 9 |
| SOURCE: N-SSATS 2013 and 2016. NOTE: Urbanicity is assigned based on the National Center for Health Statistics urbanicity classification scheme. Facilities in rural areas include those in micropolitan areas with an urban core population of at least 10,000 but less than 50,000, as well as those in non-core areas. Facilities in a central or fringe urban core with a population of 50,000 or more are considered urban. Information on urbanicity was not available for all facilities; urban and rural data are only reported for facilities with known urbanicity. Facility operation was self-designated in N-SSATS Question 7. Facility focus was not asked on the N-SSATS 2013 survey. |
||||||||||||
| TABLE B.16. Number and Percentage of Facilities Providing Any Pharmacotherapy or Opioid-Related Pharmacotherapy, by State, 2013 and 2016 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of Facilities | Percentage of Facilities | |||||||||||
| Providing Pharmacotherapies for Opioid Disorders |
Providing Any Pharmacotherapies |
Providing Pharmacotherapies for Opioid Disorders |
Providing Any Pharmacotherapies |
|||||||||
| 2013 | 2016 | Change | 2013 | 2016 | Change | 2013 | 2016 | Change | 2013 | 2016 | Change | |
| Total | 4,246 | 5,373 | 27 | 5,267 | 6,191 | 18 | 30 | 37 | 24 | 37 | 43 | 15 |
| Alabama | 49 | 52 | 6 | 53 | 57 | 8 | 32 | 38 | 20 | 34 | 42 | 22 |
| Alaska | 16 | 17 | 6 | 22 | 23 | 5 | 17 | 18 | 5 | 24 | 24 | 3 |
| Arizona | 113 | 143 | 27 | 134 | 165 | 23 | 36 | 40 | 11 | 43 | 46 | 8 |
| Arkansas | 15 | 17 | 13 | 23 | 20 | -13 | 17 | 15 | -11 | 26 | 18 | -32 |
| California | 424 | 477 | 13 | 468 | 517 | 10 | 27 | 33 | 22 | 30 | 36 | 20 |
| Colorado | 104 | 113 | 9 | 251 | 216 | -14 | 21 | 28 | 33 | 51 | 54 | 5 |
| Connecticut | 81 | 115 | 42 | 125 | 142 | 14 | 38 | 51 | 34 | 59 | 63 | 8 |
| Delaware | 18 | 28 | 56 | 18 | 29 | 61 | 43 | 60 | 39 | 43 | 62 | 44 |
| District of Columbia | 14 | 16 | 14 | 15 | 16 | 7 | 38 | 47 | 24 | 41 | 47 | 16 |
| Florida | 171 | 286 | 67 | 211 | 312 | 48 | 27 | 40 | 45 | 34 | 44 | 28 |
| Georgia | 89 | 115 | 29 | 133 | 142 | 7 | 25 | 37 | 48 | 37 | 45 | 22 |
| Hawaii | 13 | 16 | 23 | 16 | 19 | 19 | 11 | 9 | -13 | 13 | 11 | -16 |
| Idaho | 21 | 27 | 29 | 23 | 32 | 39 | 18 | 19 | 5 | 20 | 22 | 14 |
| Illinois | 165 | 189 | 15 | 198 | 208 | 5 | 25 | 28 | 10 | 30 | 31 | 1 |
| Indiana | 60 | 83 | 38 | 94 | 101 | 7 | 22 | 31 | 44 | 34 | 38 | 12 |
| Iowa | 24 | 34 | 42 | 33 | 48 | 45 | 17 | 21 | 25 | 23 | 29 | 28 |
| Kansas | 33 | 35 | 6 | 45 | 58 | 29 | 16 | 17 | 11 | 21 | 29 | 35 |
| Kentucky | 68 | 94 | 38 | 82 | 104 | 27 | 21 | 26 | 25 | 25 | 29 | 15 |
| Louisiana | 37 | 50 | 35 | 56 | 70 | 25 | 22 | 32 | 43 | 34 | 45 | 32 |
| Maine | 56 | 62 | 11 | 66 | 66 | 0 | 25 | 27 | 7 | 30 | 29 | -3 |
| Maryland | 157 | 199 | 27 | 169 | 208 | 23 | 44 | 50 | 14 | 47 | 52 | 10 |
| Massachusetts | 155 | 220 | 42 | 181 | 246 | 36 | 49 | 62 | 26 | 57 | 69 | 21 |
| Michigan | 118 | 126 | 7 | 165 | 173 | 5 | 24 | 26 | 9 | 34 | 36 | 7 |
| Minnesota | 74 | 98 | 32 | 101 | 119 | 18 | 21 | 26 | 27 | 29 | 32 | 13 |
| Mississippi | 23 | 19 | -17 | 30 | 26 | -13 | 23 | 20 | -12 | 30 | 27 | -8 |
| Missouri | 110 | 129 | 17 | 115 | 138 | 20 | 43 | 45 | 6 | 45 | 48 | 8 |
| Montana | 19 | 18 | -5 | 27 | 26 | -4 | 26 | 28 | 7 | 38 | 41 | 8 |
| Nebraska | 21 | 27 | 29 | 28 | 37 | 32 | 18 | 20 | 8 | 25 | 27 | 11 |
| Nevada | 26 | 33 | 27 | 29 | 39 | 34 | 32 | 41 | 29 | 36 | 49 | 36 |
| New Hampshire | 17 | 38 | 124 | 20 | 40 | 100 | 31 | 59 | 92 | 36 | 63 | 72 |
| New Jersey | 131 | 158 | 21 | 147 | 184 | 25 | 35 | 43 | 21 | 40 | 50 | 26 |
| New Mexico | 32 | 44 | 38 | 43 | 61 | 42 | 23 | 29 | 24 | 31 | 40 | 28 |
| New York | 510 | 661 | 30 | 574 | 692 | 21 | 56 | 72 | 27 | 63 | 75 | 18 |
| North Carolina | 131 | 169 | 29 | 159 | 195 | 23 | 30 | 35 | 14 | 37 | 40 | 9 |
| North Dakota | 9 | 10 | 11 | 18 | 18 | 0 | 14 | 17 | 20 | 28 | 30 | 8 |
| Ohio | 114 | 184 | 61 | 142 | 202 | 42 | 30 | 45 | 50 | 38 | 50 | 32 |
| Oklahoma | 26 | 38 | 46 | 34 | 52 | 53 | 12 | 19 | 60 | 15 | 25 | 67 |
| Oregon | 42 | 61 | 45 | 56 | 71 | 27 | 17 | 27 | 60 | 23 | 32 | 40 |
| Pennsylvania | 194 | 262 | 35 | 236 | 283 | 20 | 36 | 50 | 38 | 44 | 54 | 22 |
| Puerto Rico | 39 | 37 | -5 | 44 | 41 | -7 | 24 | 26 | 8 | 27 | 29 | 6 |
| Rhode Island | 32 | 39 | 22 | 40 | 42 | 5 | 52 | 75 | 45 | 65 | 81 | 25 |
| South Carolina | 35 | 37 | 6 | 38 | 41 | 8 | 32 | 32 | 3 | 34 | 36 | 5 |
| South Dakota | 7 | 13 | 86 | 13 | 16 | 23 | 11 | 21 | 89 | 21 | 26 | 25 |
| Tennessee | 57 | 85 | 49 | 74 | 94 | 27 | 26 | 37 | 45 | 33 | 41 | 24 |
| Texas | 161 | 175 | 9 | 170 | 189 | 11 | 35 | 36 | 3 | 37 | 39 | 5 |
| Utah | 64 | 112 | 75 | 73 | 125 | 71 | 37 | 48 | 27 | 43 | 53 | 25 |
| Vermont | 24 | 32 | 33 | 27 | 34 | 26 | 55 | 70 | 28 | 61 | 74 | 20 |
| Virginia | 82 | 94 | 15 | 119 | 121 | 2 | 36 | 41 | 13 | 53 | 53 | 0 |
| Washington | 84 | 96 | 14 | 94 | 110 | 17 | 19 | 22 | 20 | 21 | 26 | 23 |
| West Virginia | 47 | 57 | 21 | 57 | 62 | 9 | 47 | 54 | 16 | 56 | 58 | 4 |
| Wisconsin | 113 | 106 | -6 | 152 | 130 | -14 | 36 | 38 | 7 | 48 | 46 | -3 |
| Wyoming | 19 | 24 | 26 | 23 | 28 | 22 | 36 | 41 | 15 | 43 | 48 | 11 |
| Other US Territories | 2 | 3 | 50 | 3 | 3 | 0 | 22 | 30 | 35 | 33 | 30 | -10 |
| SOURCE: N-SSATS 2013 and 2016. | ||||||||||||
| TABLE B.17. Number and Percentage Change in Residential and Inpatient-Designated Beds and Utilization Rate by State, 2013 and 2015 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of Designated Beds | Utilization Rate | |||||||||||
| Residential | Inpatient Hospital | Residential | Inpatient Hospital | |||||||||
| 2013 | 2015 | Change | 2013 | 2015 | Change | 2013 | 2015 | Change | 2013 | 2015 | Change | |
| Total | 100,417 | 104,012 | 4 | 12,213 | 15,415 | 26 | 97 | 105 | 9 | 97 | 109 | 12 |
| Alabama | 1,212 | 1,031 | -15 | 252 | 52 | -79 | 92 | 95 | 3 | 96 | 54 | -44 |
| Alaska | 383 | 347 | -9 | NA | NA | NA | 89 | 109 | 23 | NA | 0- | NA |
| Arizona | 1,853 | 2,235 | 21 | 210 | 297 | 41 | 97 | 120 | 23 | 129 | 117 | -9 |
| Arkansas | 798 | 686 | -14 | 83 | 46 | -45 | 86 | 350 | 308 | 94 | 63 | -33 |
| California | 13,688 | 13,390 | -2 | 750 | 477 | -36 | 94 | 95 | 1 | 102 | 95 | -7 |
| Colorado | 1,446 | 1,162 | -20 | 172 | 184 | 7 | 97 | 93 | -5 | 80 | 73 | -9 |
| Connecticut | 1,766 | 1,491 | -16 | 290 | 219 | -24 | 100 | 101 | 0 | 98 | 111 | 13 |
| Delaware | 184 | 262 | 42 | NA | 30 | NA | 92 | 1450 | 1,470 | NA | 107 | NA |
| District of Columbia | 428 | 396 | -7 | NA | 12 | NA | 98 | 109 | 11 | NA | 8 | NA |
| Florida | 6,020 | 6,363 | 6 | 641 | 843 | 32 | 120 | 101 | -16 | 94 | 128 | 36 |
| Georgia | 1,934 | 1,933 | 0 | 284 | 413 | 45 | 98 | 83 | -15 | 90 | 110 | 22 |
| Hawaii | 456 | 466 | 2 | NA | 48 | NA | 84 | 95 | 12 | 0 | 92 | NA |
| Idaho | 162 | 144 | -11 | NA | 15 | NA | 70 | 97 | 39 | NA | 93 | NA |
| Illinois | 3,099 | 2,885 | -7 | 328 | 253 | -23 | 87 | 100 | 15 | 59 | 65 | 9 |
| Indiana | 541 | 618 | 14 | 237 | 552 | 133 | 82 | 130 | 59 | 75 | 92 | 24 |
| Iowa | 815 | 935 | 15 | NA | 30 | NA | 80 | 73 | -9 | NA | 80 | NA |
| Kansas | 765 | 720 | -6 | NA | 29 | NA | 85 | 96 | 12 | NA | 79 | NA |
| Kentucky | 1,798 | 2,264 | 26 | 291 | 329 | 13 | 102 | 94 | -8 | 80 | 126 | 58 |
| Louisiana | 1,615 | 1,785 | 11 | 199 | 270 | 36 | 83 | 92 | 10 | 81 | 74 | -8 |
| Maine | 296 | 257 | -13 | 112 | 118 | 5 | 107 | 91 | -15 | 108 | 39 | -64 |
| Maryland | 2,074 | 2,063 | -1 | 709 | 344 | -51 | 70 | 86 | 22 | 57 | 75 | 32 |
| Massachusetts | 3,211 | 3,292 | 3 | 595 | 811 | 36 | 95 | 105 | 11 | 106 | 121 | 14 |
| Michigan | 2,985 | 2,996 | 0 | 180 | 173 | -4 | 163 | 88 | -46 | 186 | 45 | -76 |
| Minnesota | 3,862 | 3,593 | -7 | 63 | 95 | 51 | 96 | 93 | -4 | 92 | 76 | -18 |
| Mississippi | 1,133 | 968 | -15 | 259 | 148 | -43 | 71 | 69 | -3 | 129 | 128 | 0 |
| Missouri | 1,107 | 1,215 | 10 | 55 | 73 | 33 | 88 | 175 | 99 | 195 | 77 | -61 |
| Montana | 258 | 222 | -14 | 24 | 78 | 225 | 177 | 84 | -52 | 529 | 118 | -78 |
| Nebraska | 812 | 748 | -8 | NA | NA | NA | 82 | 98 | 20 | 0 | 0 | 0 |
| Nevada | 455 | 543 | 19 | 113 | 143 | 27 | 93 | 90 | -4 | 131 | 133 | 1 |
| New Hampshire | 368 | 390 | 6 | NA | 15 | NA | 90 | 90 | 0 | NA | 27 | NA |
| New Jersey | 2,541 | 2,837 | 12 | 365 | 307 | -16 | 105 | 118 | 12 | 95 | 131 | 37 |
| New Mexico | 481 | 483 | 0 | 137 | 125 | -9 | 353 | 83 | -77 | 72 | 90 | 25 |
| New York | 10,531 | 10,125 | -4 | 2,067 | 1,741 | -16 | 91 | 97 | 7 | 79 | 95 | 20 |
| North Carolina | 2,655 | 2,591 | -2 | 429 | 368 | -14 | 92 | 112 | 21 | 129 | 73 | -44 |
| North Dakota | 378 | 440 | 16 | 94 | 83 | -12 | 111 | 84 | -25 | 56 | 71 | 26 |
| Ohio | 1,758 | 1,955 | 11 | 586 | 561 | -4 | 99 | 102 | 3 | 84 | 88 | 4 |
| Oklahoma | 1,570 | 1,206 | -23 | 131 | 113 | -14 | 76 | 97 | 27 | 85 | 68 | -20 |
| Oregon | 1,260 | 1,268 | 1 | 83 | 52 | -37 | 85 | 97 | 15 | 75 | 185 | 147 |
| Pennsylvania | 5,756 | 5,570 | -3 | 529 | 392 | -26 | 91 | 95 | 4 | 83 | 62 | -25 |
| Puerto Rico | 3,027 | 2,553 | -16 | 178 | 198 | 11 | 75 | 109 | 44 | 251 | 178 | -29 |
| Rhode Island | 348 | 1,721 | 395 | NA | 3,543 | NA | 93 | 100 | 8 | NA | 100 | NA |
| South Carolina | 471 | 692 | 47 | 301 | 209 | -31 | 117 | 89 | -24 | 116 | 537 | 364 |
| South Dakota | 543 | 623 | 15 | 87 | 98 | 13 | 115 | 93 | -19 | 86 | 69 | -19 |
| Tennessee | 1,848 | 1,913 | 4 | 142 | 129 | -9 | 86 | 93 | 8 | 280 | 95 | -66 |
| Texas | 5,448 | 4,809 | -12 | 375 | 404 | 8 | 87 | 122 | 40 | 89 | 138 | 56 |
| Utah | 896 | 928 | 4 | NA | 49 | NA | 109 | 91 | -17 | NA | 71 | NA |
| Vermont | 245 | 213 | -13 | 112 | 116 | 4 | 404 | 77 | -81 | 82 | 587 | 615 |
| Virginia | 801 | 1,060 | 32 | 109 | 277 | 154 | 72 | 95 | 32 | 152 | 113 | -26 |
| Washington | 2,417 | 5,729 | 137 | 189 | 192 | 2 | 87 | 117 | 35 | 72 | 77 | 6 |
| West Virginia | 433 | 552 | 27 | NA | 74 | NA | 91 | 93 | 2 | NA | 55 | NA |
| Wisconsin | 1,114 | 904 | -19 | 130 | 261 | 101 | 74 | 86 | 17 | 102 | 68 | -33 |
| Wyoming | 316 | 388 | 23 | NA | 16 | NA | 103 | 83 | -20 | 0 | 31 | NA |
| US territories | 56 | 52 | -7 | NA | 10 | NA | 89 | 83 | -7 | 0 | 240 | NA |
| SOURCE: N-SSATS 2013 Questions 28d and 29d, and N-SSATS 2015, Questions 29d and 30d, indicate hospital-designated and residential-designated beds. NOTE: Utilization rate is calculated by dividing the number of clients in care by the total number of designated beds. |
||||||||||||
PROJECT AND REPORT INFORMATION
Examining Substance Use Disorder Treatment Demand and Provider Capacity in a Changing Health Care System
This report was prepared under contract #HHSP23320100019WI between the U.S. Department of Health and Human Services (HHS), Office of Disability, Aging and Long-Term Care Policy (DALTCP) and Mathematica Policy Research. For additional information about this subject, you can visit the DALTCP home page at http://aspe.hhs.gov/office-disability-aging-and-long-term-care-policy-daltcp or contact the ASPE Project Officer, Judith Dey, at HHS/ASPE/DALTCP, Room 424E, H.H. Humphrey Building, 200 Independence Avenue, S.W., Washington, D.C. 20201. Her e-mail addresses is: Judith.Dey@hhs.gov.
-
Examining Substance Use Disorder Treatment Demand and Provider Capacity in a Changing Health Care System: Initial Findings Report
-
Examining Substance Use Disorder Treatment Demand and Provider Capacity in a Changing Health Care System: Final Report
-
Substance Use Disorder Workforce Issue Brief
